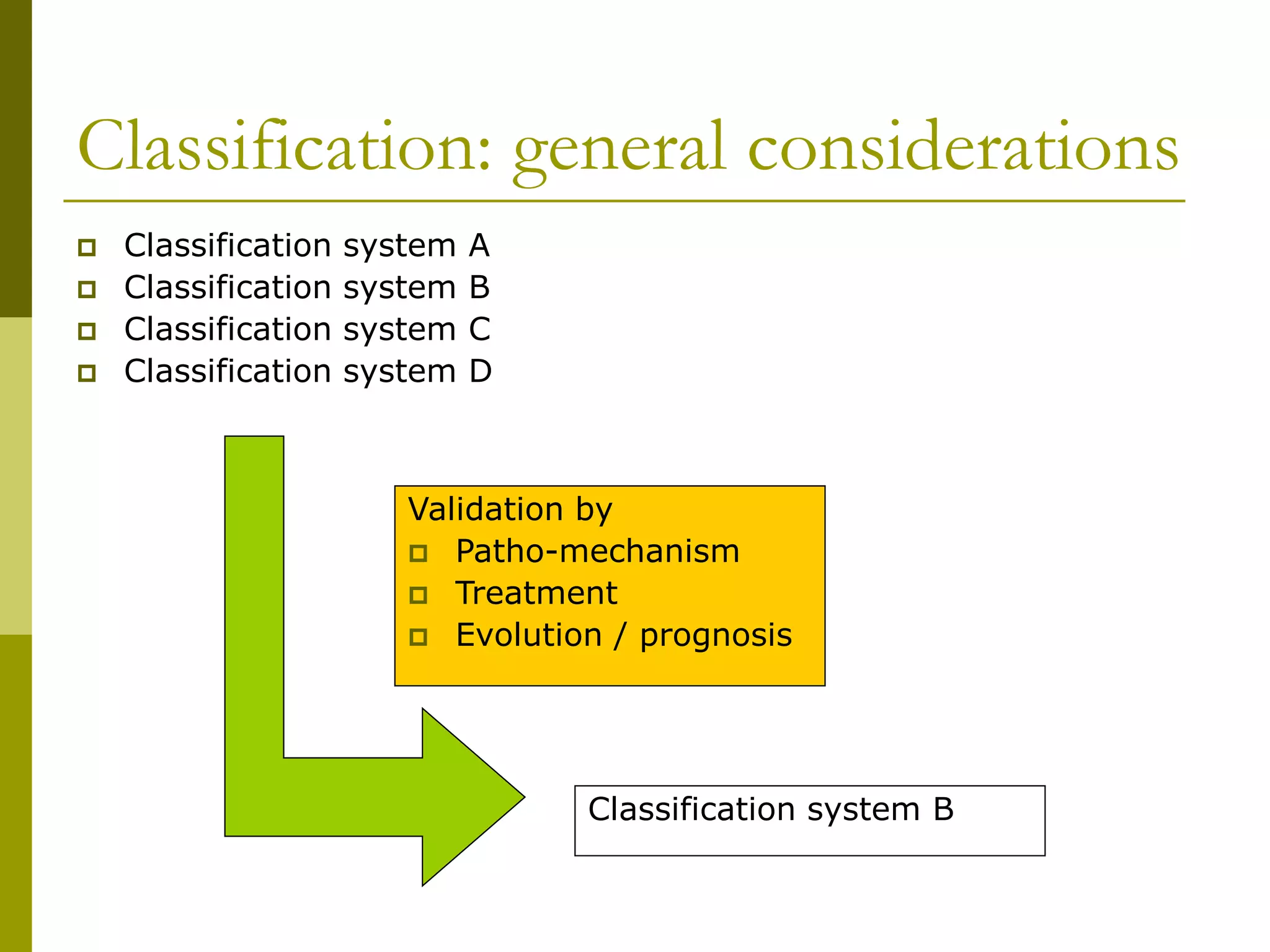
The document provides a comprehensive overview of vitiligo, including its clinical classification, subtypes (non-segmental and segmental), and associated diseases. It discusses the challenges in defining and assessing vitiligo, the absence of consensus in classification systems, and various methods of assessing disease activity. It emphasizes that predicting future evolution and localization remains difficult due to the complexity and variability of vitiligo.