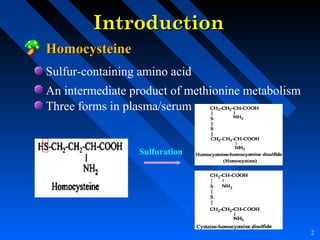
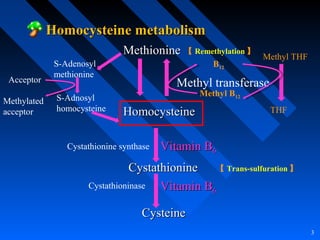
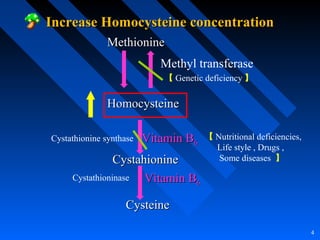
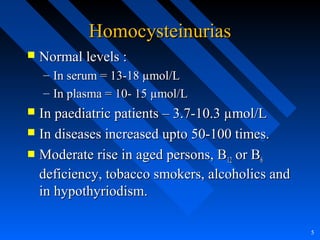
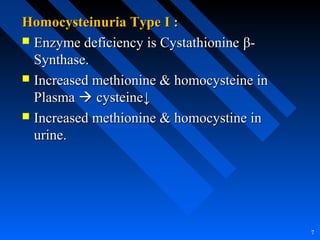
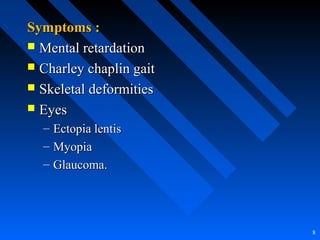
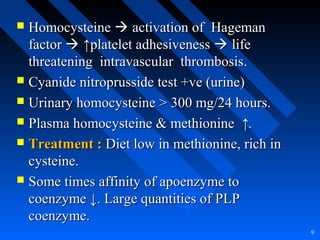
Homocysteine is a sulfur-containing amino acid and intermediate product of methionine metabolism. It exists in three forms in plasma/serum and is involved in two metabolic pathways - remethylation and trans-sulfuration. Genetic or acquired deficiencies in enzymes and vitamins involved in homocysteine metabolism can lead to hyperhomocysteinemia, which is associated with various diseases like cardiovascular disorders. Laboratory tests are available to measure homocysteine levels to screen for deficiencies and diseases. Elevated homocysteine promotes oxidative damage and impaired vascular function.