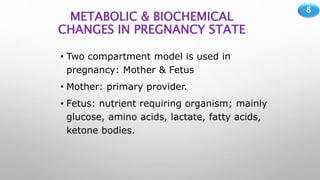
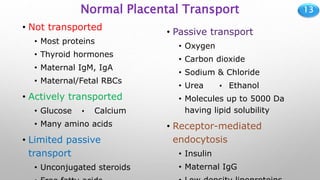
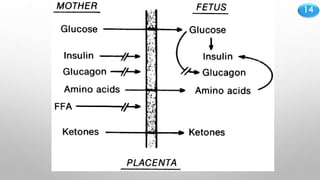
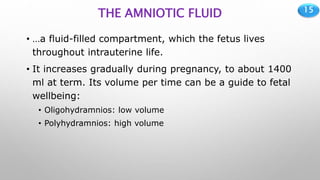
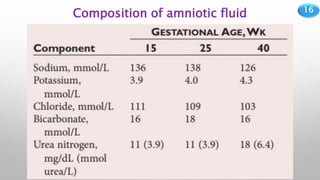
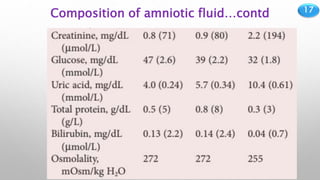
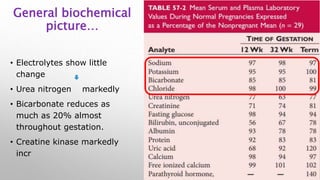
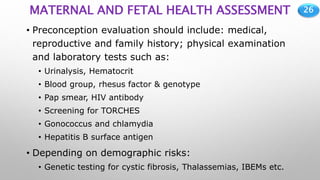
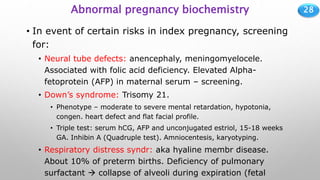
The document outlines the biochemical and physiological changes during pregnancy, including maternal and fetal adaptations, placental functions, and complications that may arise. It highlights the importance of monitoring various biochemical parameters to assess maternal and fetal health throughout the gestation period. Key topics include hormonal influences, metabolic shifts, and the assessment of potential pregnancy-related disorders.