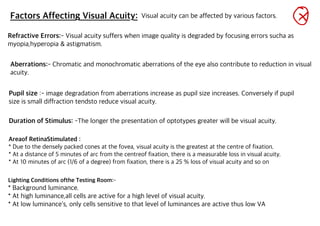
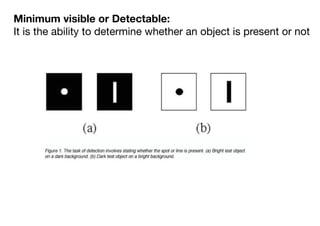
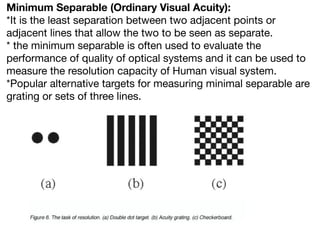
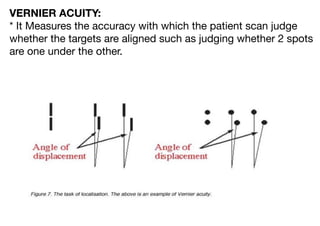
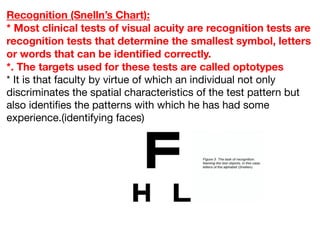
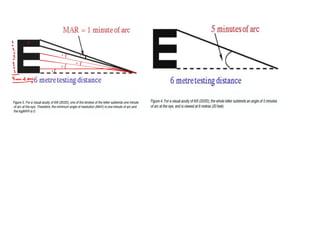
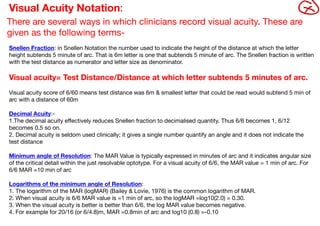
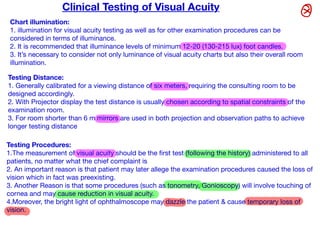
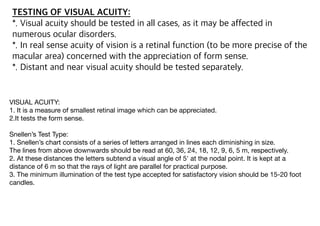
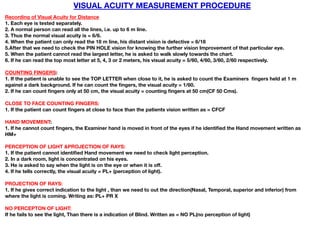
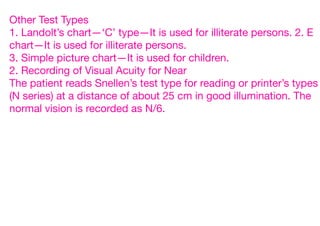
Visual acuity is a measurement of the eye's ability to resolve fine detail and discriminate spacing between objects. It is tested using optotypes of decreasing size on charts like the Snellen chart. Visual acuity can be affected by refractive errors, aberrations, pupil size, stimulus duration, and retinal location. It is measured for both distance and near vision using tests that evaluate minimum detectable, minimum separable, and Vernier acuity. Recordings include the Snellen fraction or logarithm of the minimum angle of resolution. Proper testing involves standardized illumination and procedures to accurately assess a patient's vision.