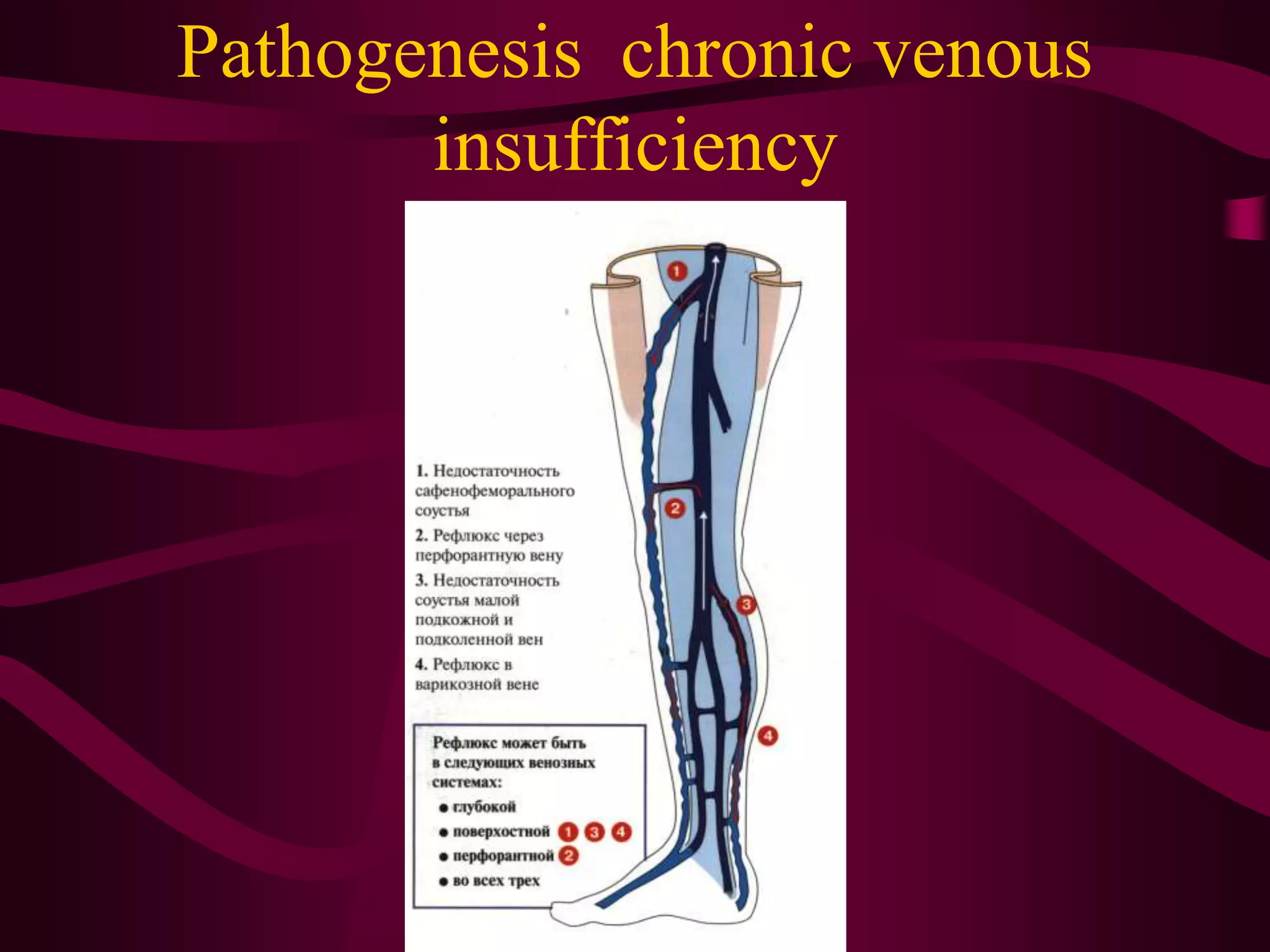
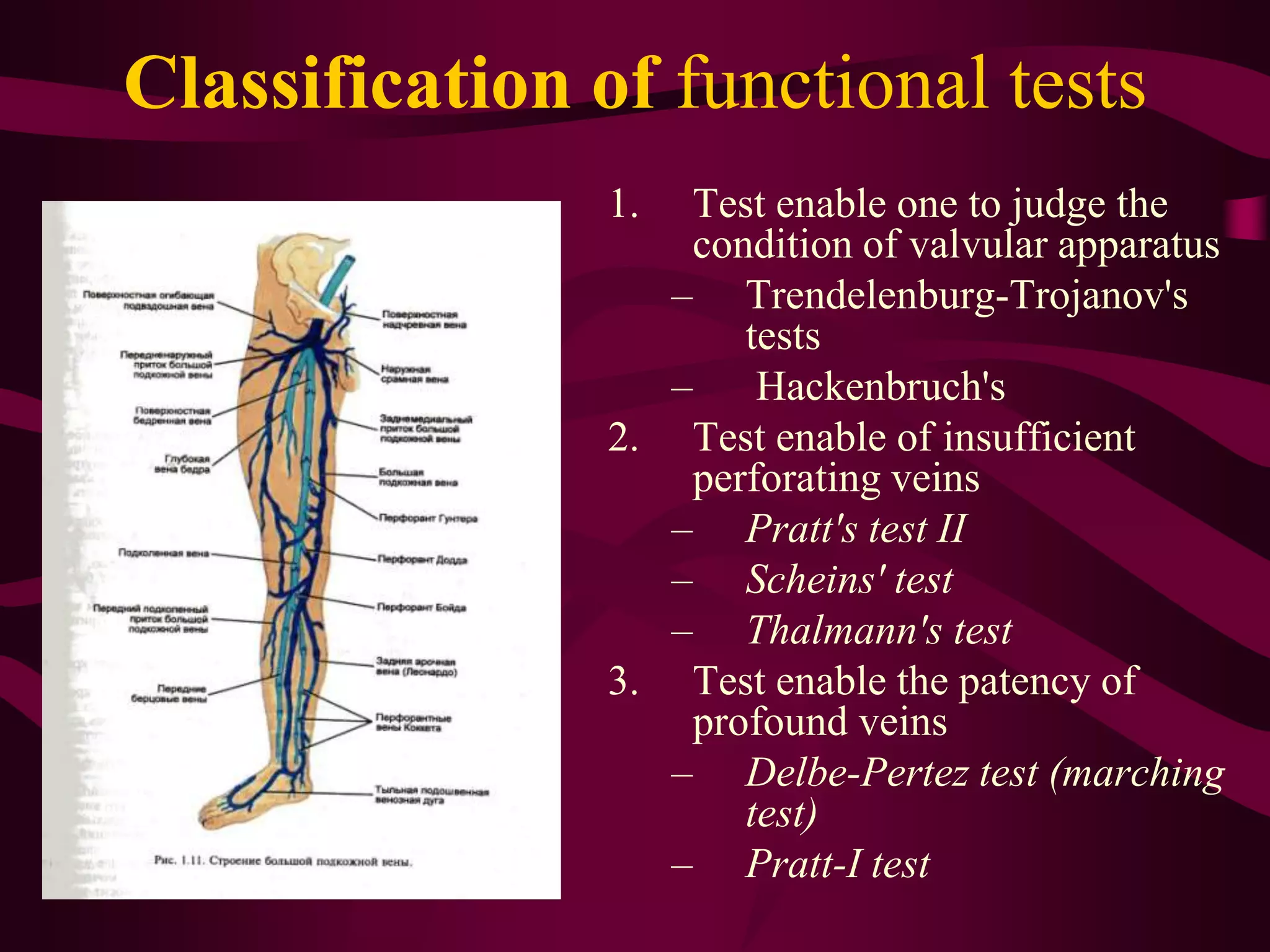
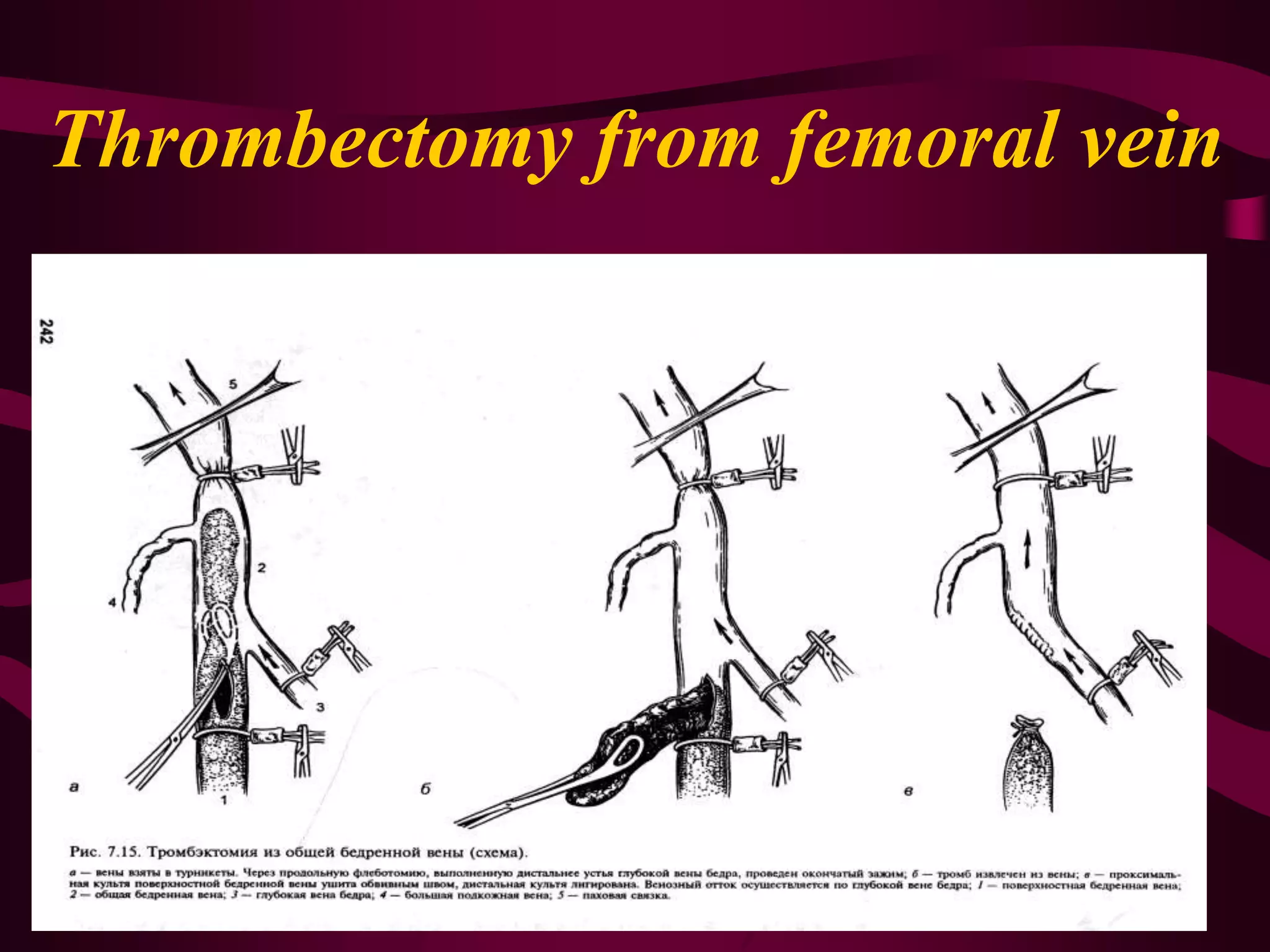
This document discusses classification and treatment of venous disorders of the extremities. It classifies diseases by location such as the superior and inferior vena cava, describes conditions like thrombophlebitis, varicose veins and post-thrombophlebitic syndrome. Diagnostic tests and stages of chronic venous insufficiency are outlined. Conservative treatments include compression therapy, medications and anticoagulants. Surgical options are described for eliminating reflux and removing varicose veins.