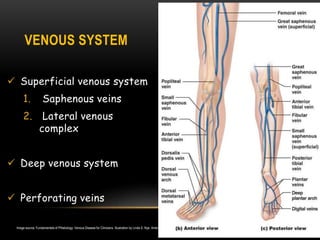
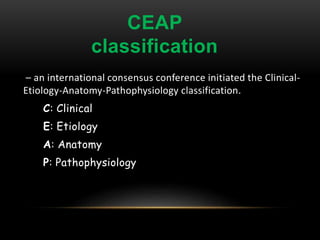
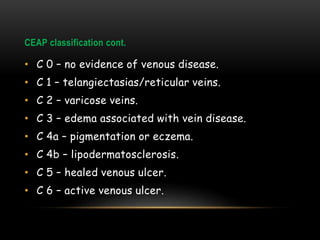
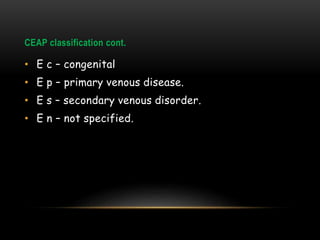
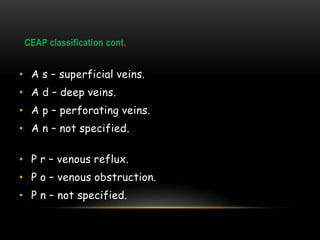
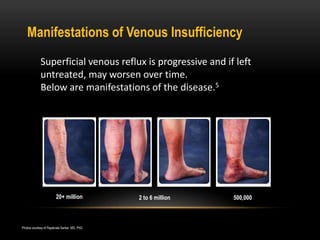
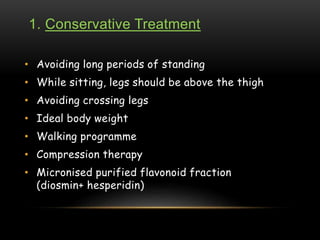
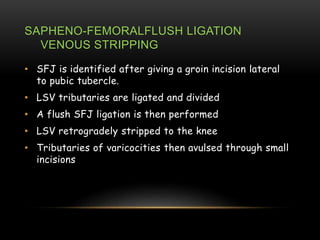
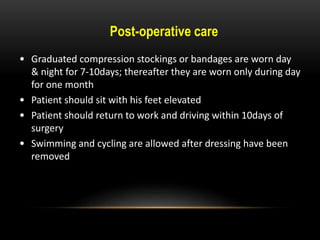
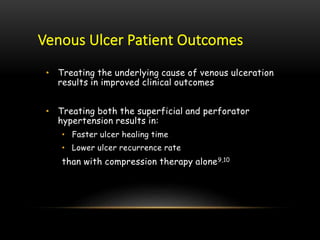
Chronic superficial venous insufficiency (CSVI) occurs when the valves in the superficial leg veins fail, leading to blood pooling in the legs and potential complications like varicose veins and venous ulcers. The CEAP classification system is used to categorize the severity of venous disease, focusing on clinical presentation, etiology, anatomy, and pathophysiology. Treatment options range from conservative measures, like compression therapy and lifestyle changes, to more invasive procedures such as vein ablation and surgical interventions.






![REFERENCES
1. American Heart Association, SIR, Brand et al. “The Epidemiology of Varicose Veins: The
Framingham Study”
2. US Markets for Varicose Vein Treatment Devices 2006, Millennium Research Group 2005.
3. Coon WW, Willis PW, Keller JB: Venous thromboembolism and other venous disease in the
Tecumseh Community Health Study Circulation 1973; 48:839-846.
4. Barron HC, Ross BA. Varicose Veins: A guide to prevention and treatment. NY, NY: Facts on File, Inc.
[An Infobase Holdings Company]; 1995;vii.
5. White JV, Ryjewski C. Chronic venous insufficiency. Perspect Vasc Surg Endovasc Ther 2005;17:319-
27
6. Dietzek A, Two-Year Follow-Up Data From A Prospective, Multicenter Study Of The Efficacy Of The
ClosureFAST Catheter, 35th Annual Veith Symposium. November 19, 2008. New York.
7. Alameida JI. Lessons Learned After 2000 Endovenous Ablations. 34th Veith Symposium. Nov 14-18,
2007. New York
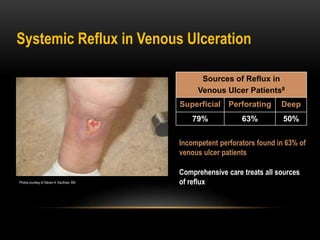
8. Hanrahn L. et al. Distribution of valvular incompetence in patients with venous stasis ulceration.
JVS 13,6, 805-812 June 1991
9. Jamie R Barwell, Colin E Davies, Comparison of surgery and compression with compression alone
in chronic venous ulceration (ESCHAR study): randomized controlled trial,THE LANCET, Vol 363,
June 04
10. Nelzen O. Fransson I. True long-term healing and recurrence of venous leg ulcers following SEPS
combined with superficial venous surgery: a prospective study. Eur J Vasc Endovasc Surg 34, 605-
612 (2007)](https://image.slidesharecdn.com/csvi2-160405160816/85/Chronic-Superficial-Venous-insufficiency-41-320.jpg)
