This document provides information on chronic kidney disease (CKD) and dialysis. It discusses:
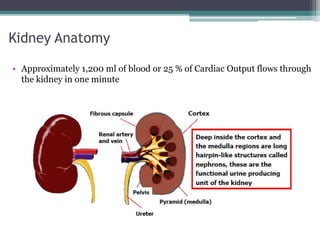
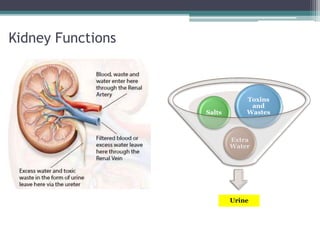
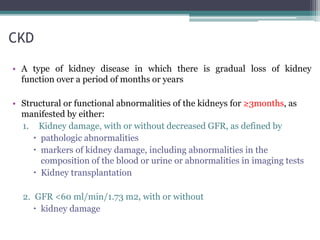
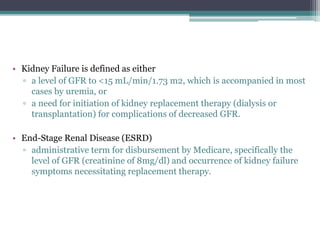
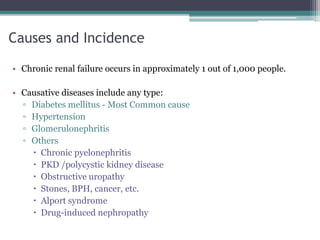
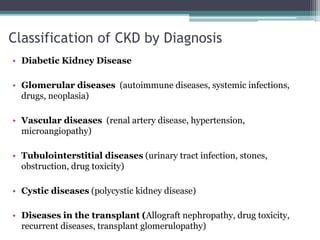
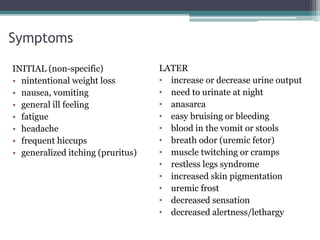
1. The functions of the kidneys and how CKD develops due to gradual loss of kidney function over time.
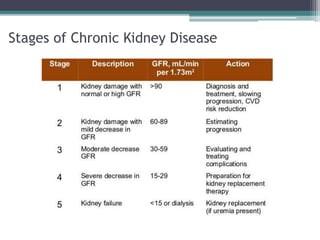
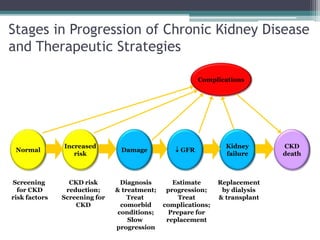
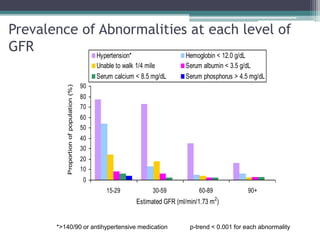
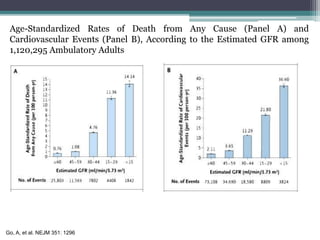
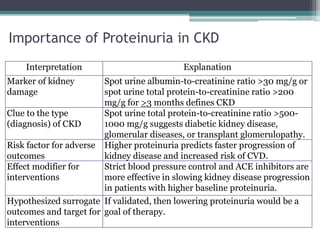
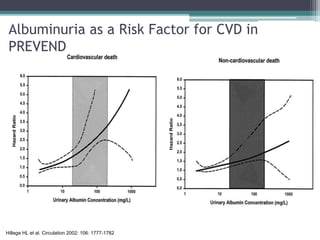
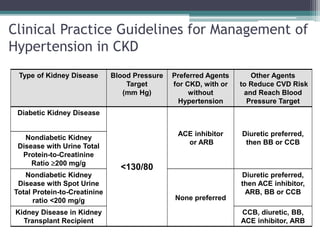
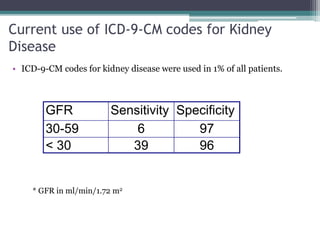
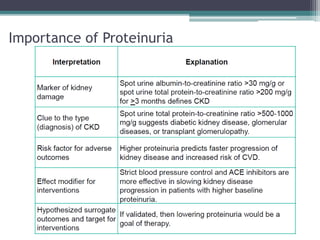
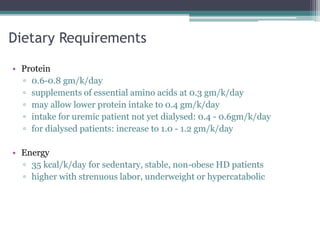
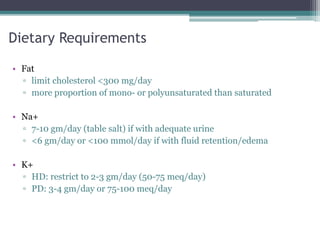
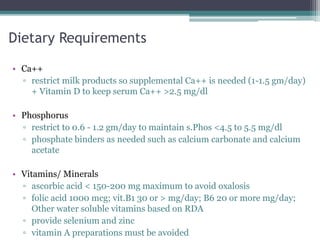
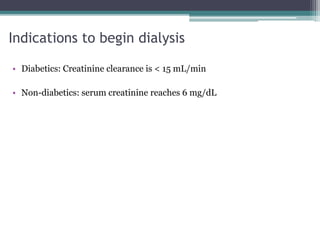
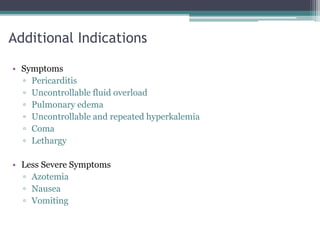
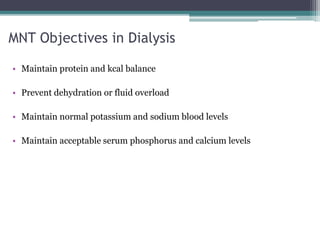
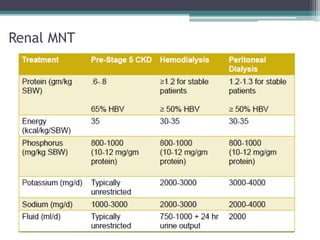
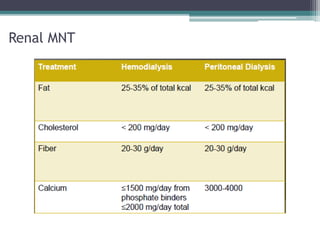
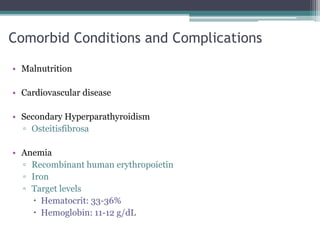
2. The stages of CKD progression and treatment strategies at each stage, including managing risk factors, complications, and preparing for renal replacement therapy.
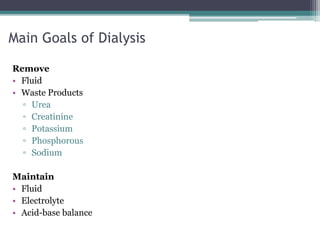
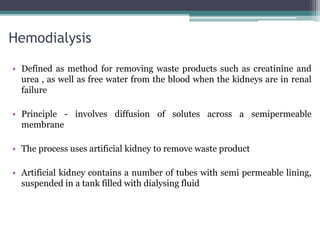
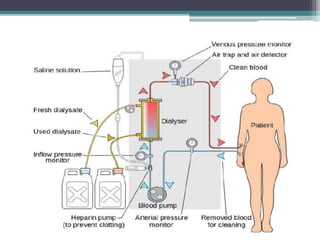
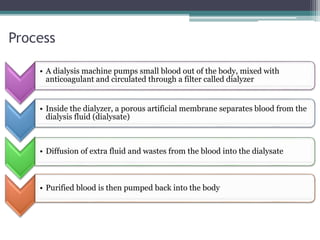
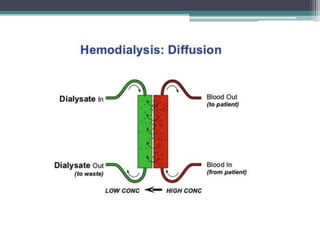
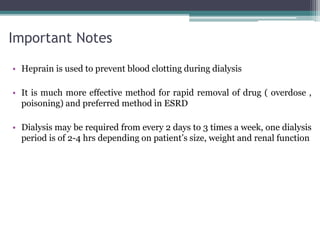
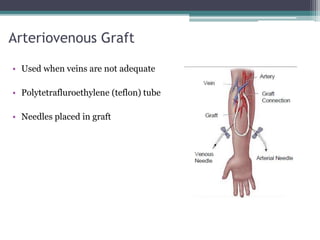
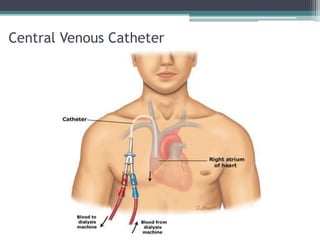
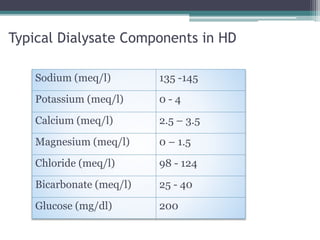
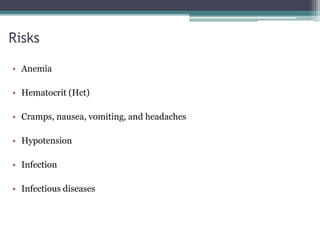
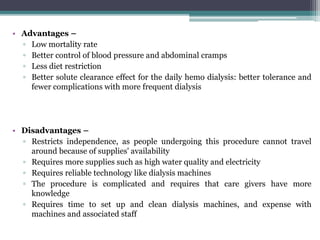
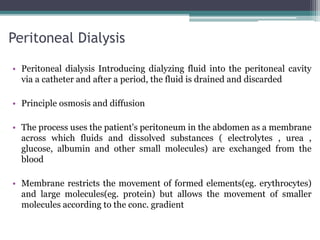
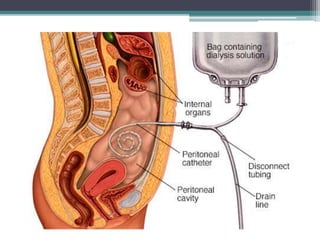
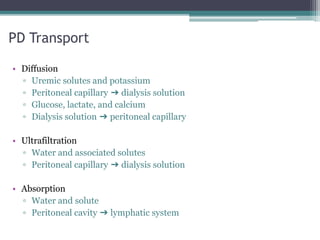
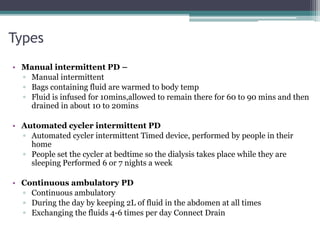
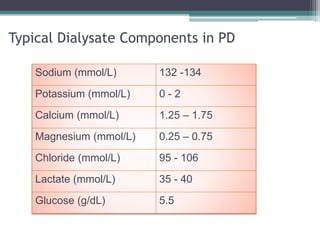
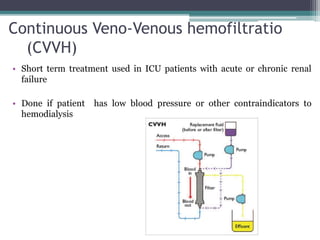
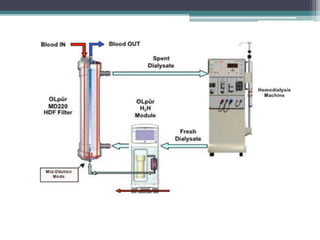
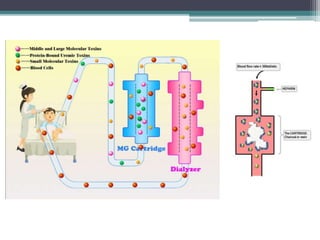
3. The two main types of renal replacement therapy - hemodialysis which uses an artificial kidney to filter waste from the blood, and peritoneal dialysis which uses the peritoneal membrane in the abdomen.