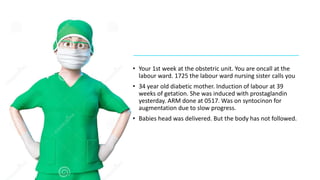
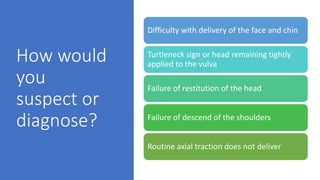
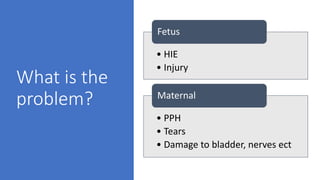
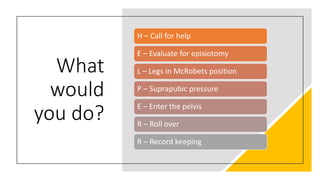
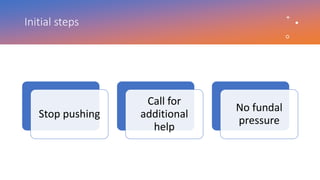
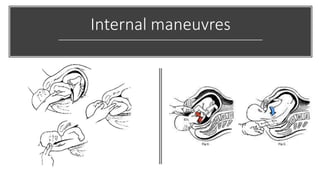
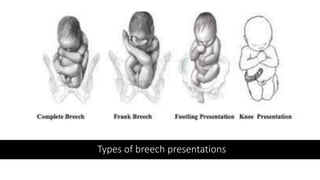
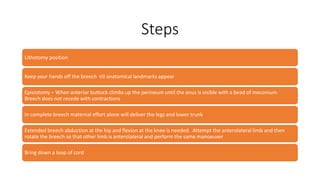
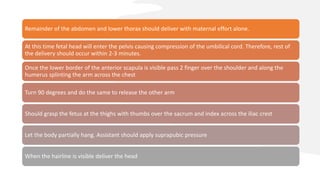
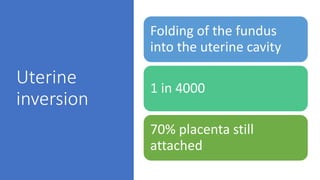
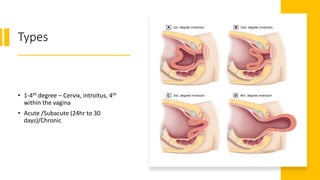
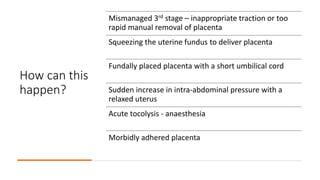
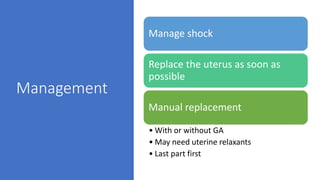
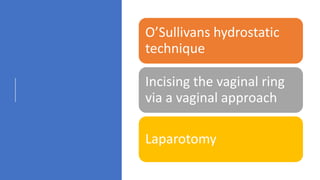
The document outlines critical management protocols for obstetric emergencies, specifically focusing on shoulder dystocia and breech delivery techniques. It details the diagnostic signs and necessary maneuvers, such as the McRoberts position and suprapubic pressure, while emphasizing the importance of record-keeping and medico-legal considerations. Additionally, it discusses uterine inversion, its causes, and management strategies, including manual replacement techniques.