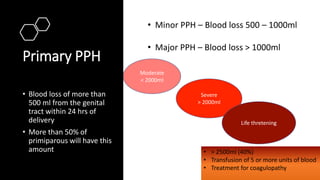
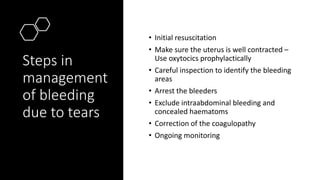
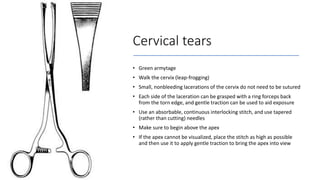
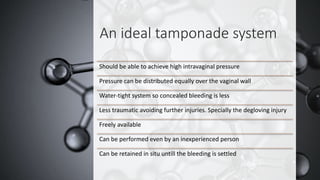
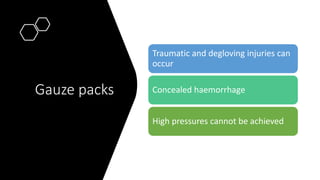
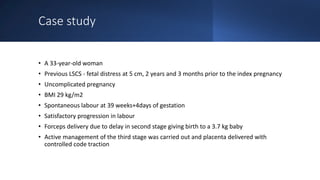
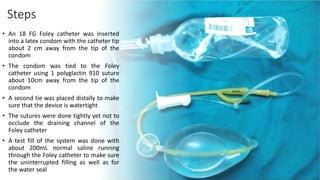
This document addresses the management of postpartum hemorrhage (PPH), detailing its classification, causes, and critical steps in managing bleeding due to tears. It emphasizes the importance of uterine atony management and describes effective techniques for suturing cervical and vaginal lacerations. A case study illustrates the challenges and outcomes of treating a patient with severe vaginal bleeding, including the successful use of a vaginal condom catheter for tamponade.