1) Uterine fibroids (leiomyomas) are benign muscle tumors that are very common in women.
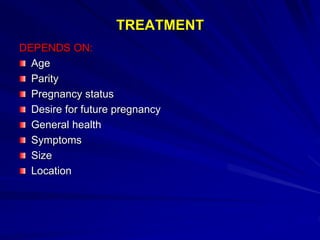
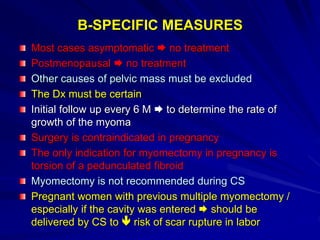
2) Treatment depends on a woman's symptoms, age, fertility desires, and size and location of the fibroids.
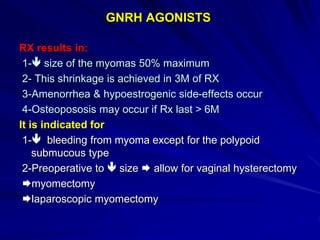
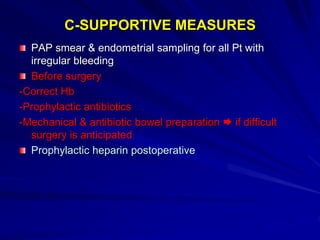
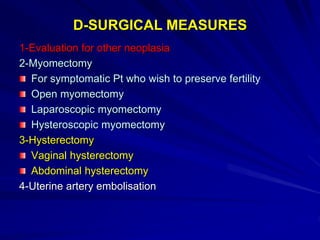
3) Options include pain management, myomectomy (surgical removal of fibroids), hysterectomy (removal of the uterus), or uterine artery embolization to reduce blood flow to the fibroids.