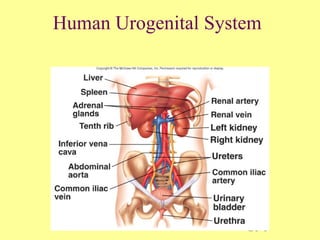
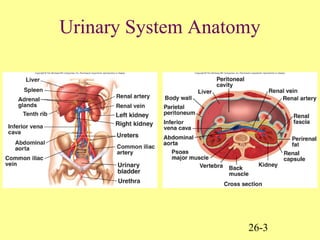
The document discusses the human urogenital system and kidney anatomy and function. It provides details on:
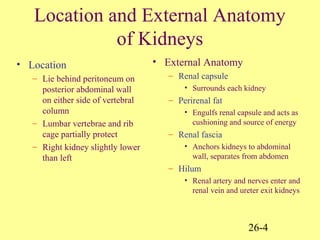
- The location and external anatomy of the kidneys in the body.
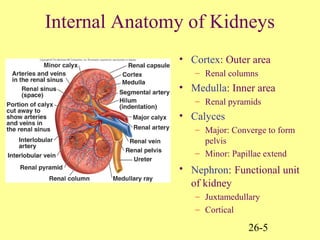
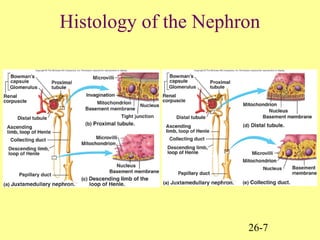
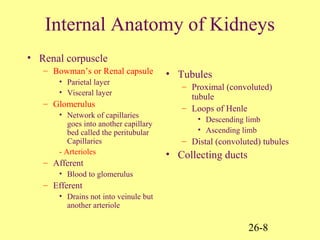
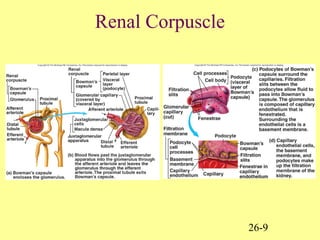
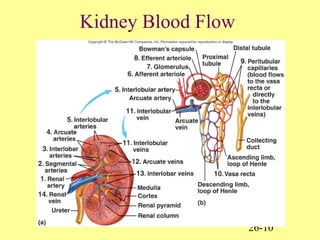
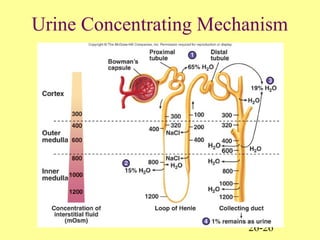
- The internal anatomy of the kidneys including nephrons, renal corpuscles, tubules, and collecting ducts.
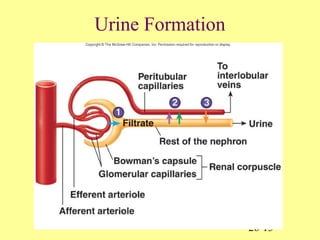
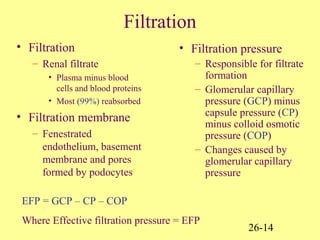
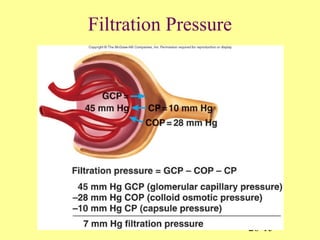
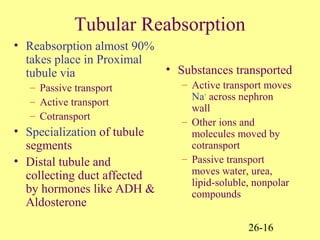
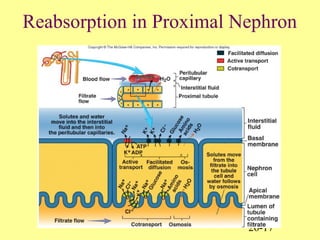
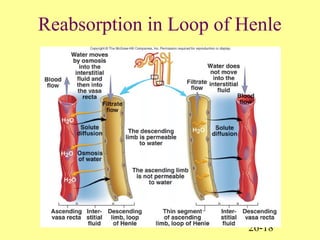
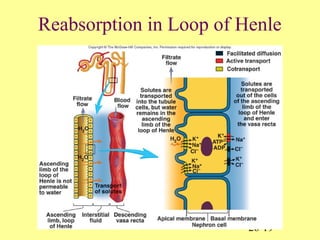
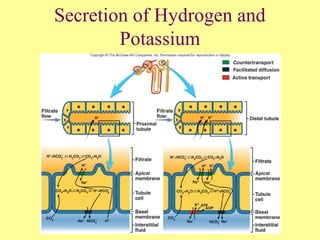
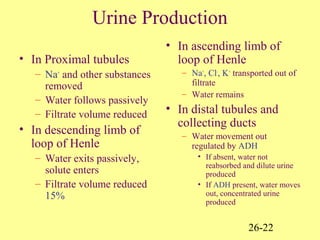
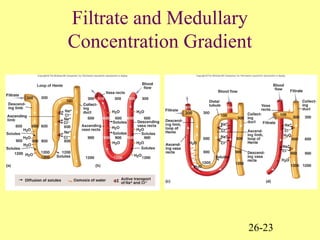
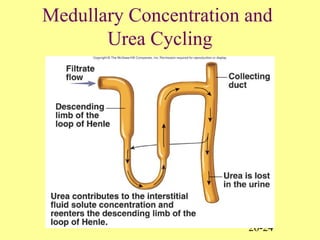
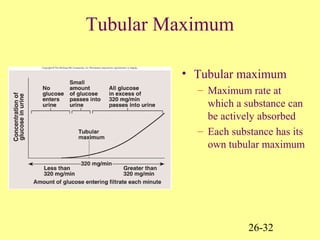
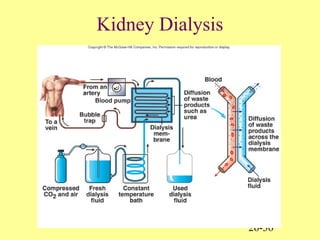
- How the kidneys filter blood to remove wastes and regulate fluid and electrolyte balance through processes like filtration, reabsorption, and secretion in the nephrons.
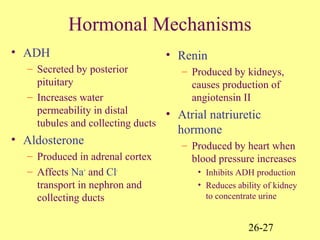
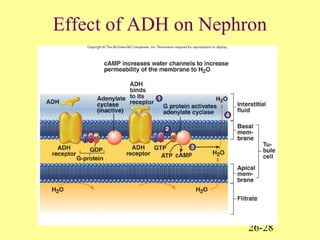
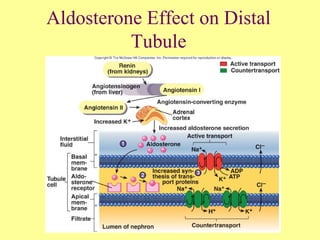
- Hormonal control of kidney functions including ADH and aldosterone.