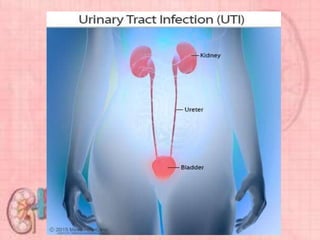
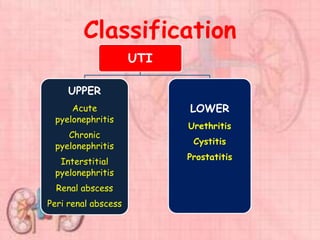
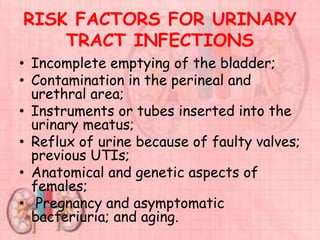
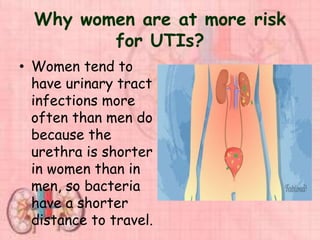
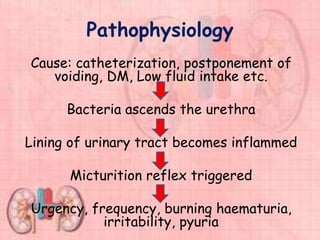
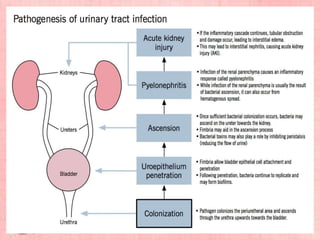
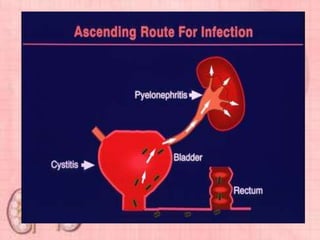
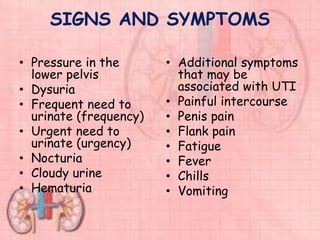
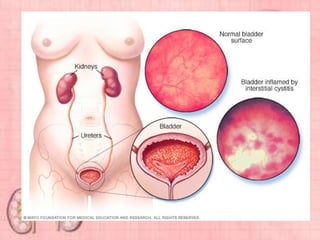
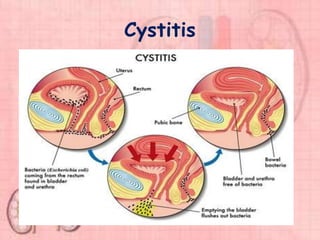
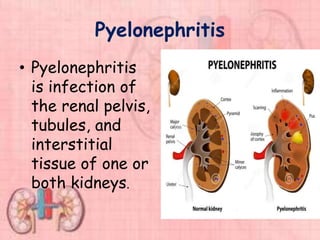
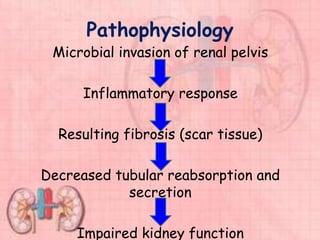
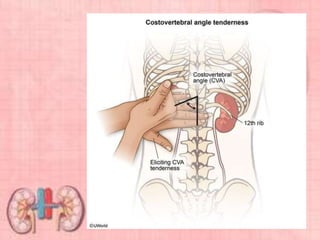
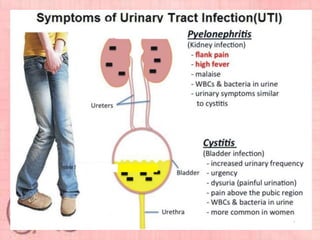
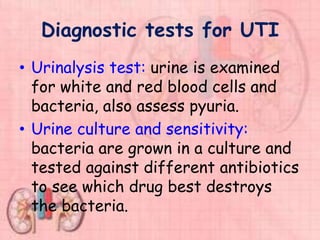
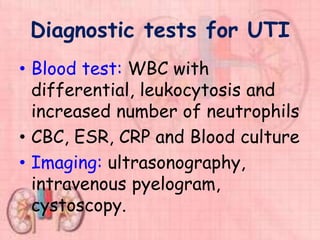
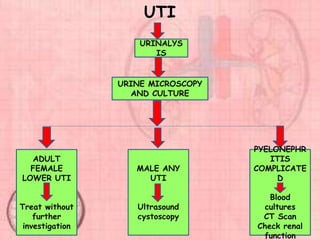
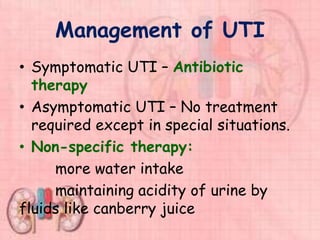
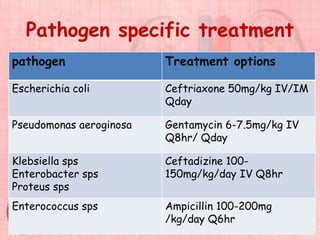
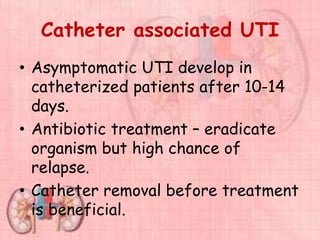
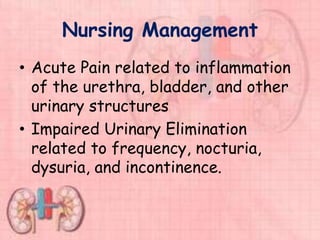
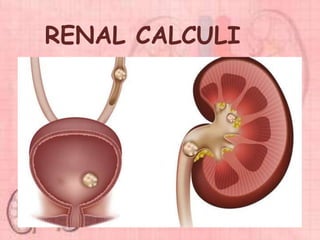
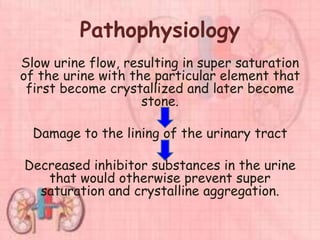
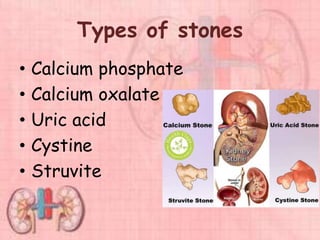
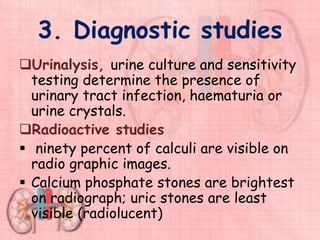
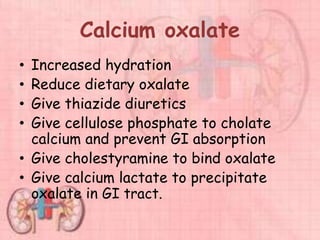
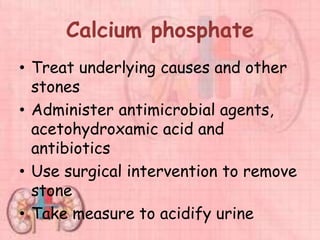
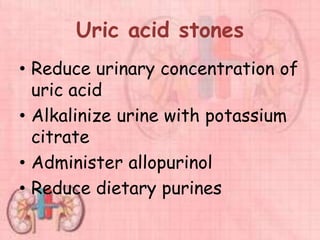
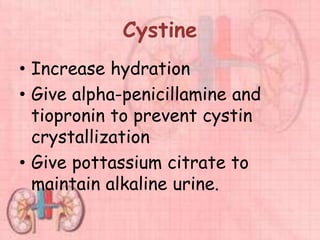
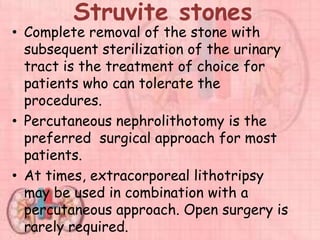
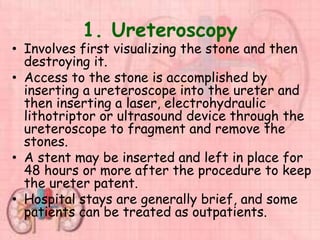
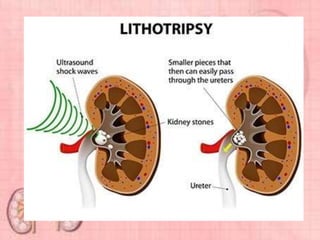
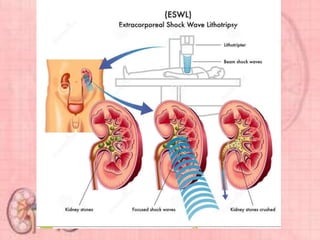
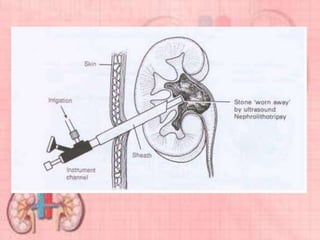
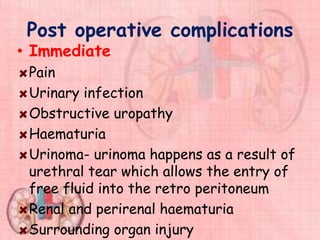
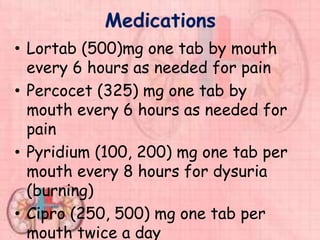
This document provides information about urinary tract infections (UTIs). It begins with an introduction to UTIs, noting they are common and usually responsive to antibiotics. The document then covers classification of UTIs, risk factors, symptoms, diagnostic tests, treatment including antibiotics, and complications. It also provides details on specific types of UTIs like cystitis, urethritis and pyelonephritis. The document concludes with a section on renal calculi/kidney stones, discussing causes, types, diagnosis and treatment.