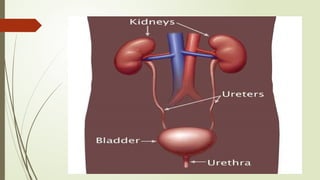
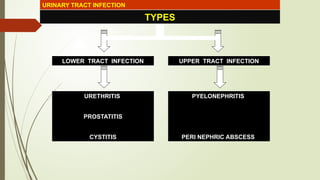
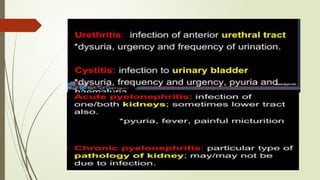
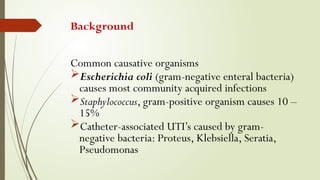
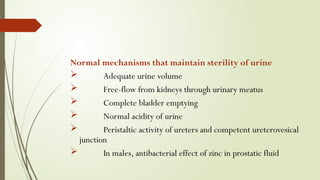
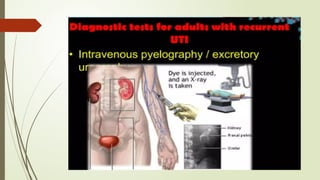
The document outlines the definition, pathophysiology, risk factors, and types of urinary tract infections (UTIs), emphasizing their prevalence and causative organisms, particularly E. coli. It details the distinctions between lower and upper tract infections, including conditions like cystitis and pyelonephritis, along with their symptoms and treatment options. Risk factors include age, gender, urinary tract obstructions, and anomalies, and the document highlights the significance of proper diagnosis and antibiotic treatment.