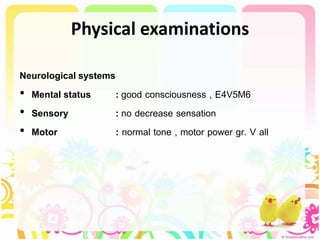
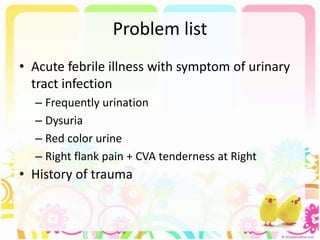
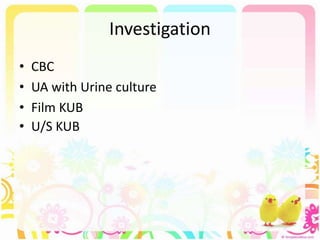
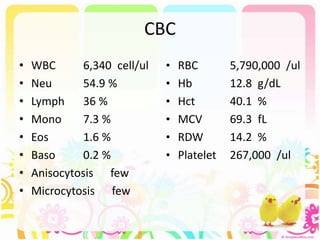
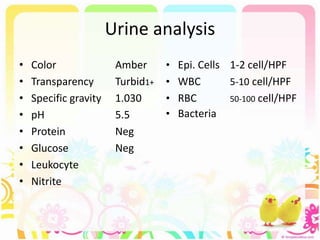
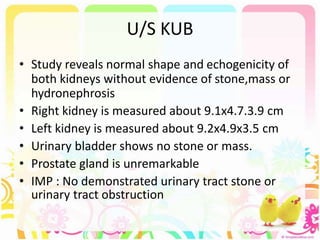
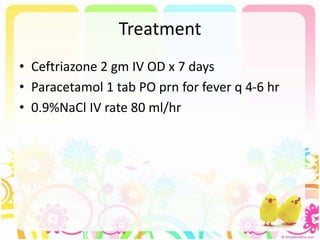
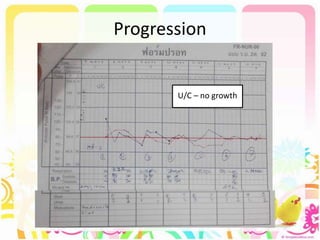
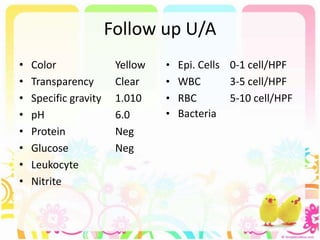
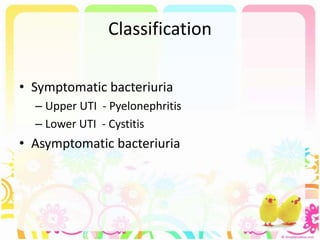
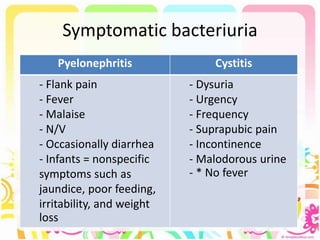
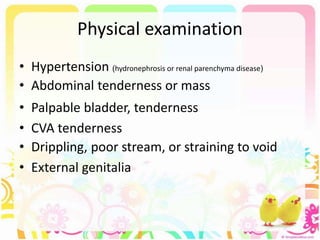
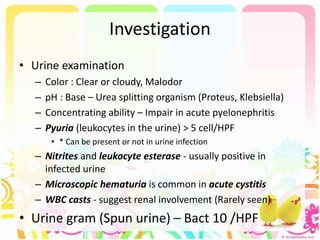
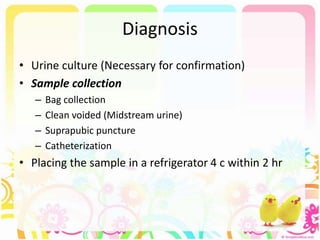
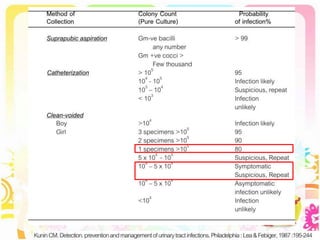
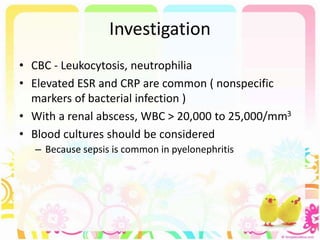
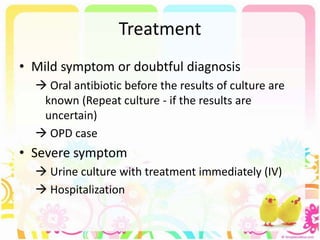
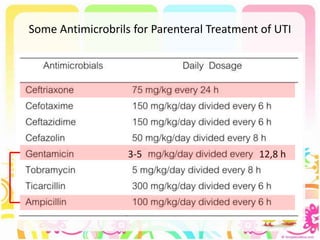
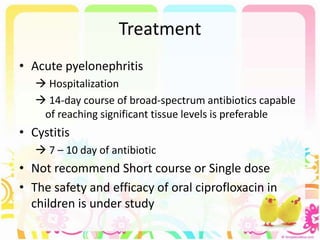
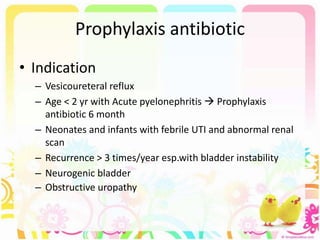
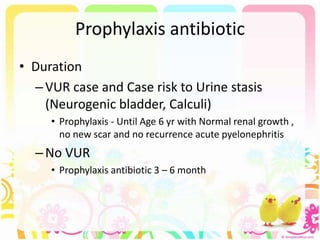
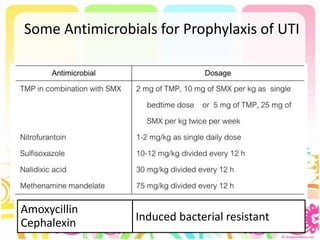
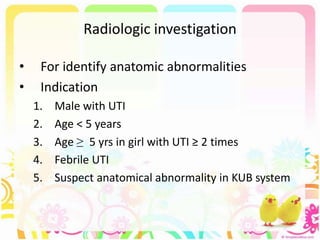
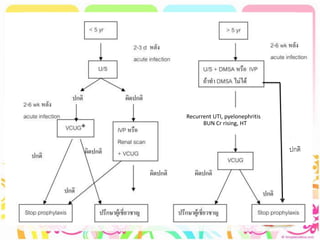
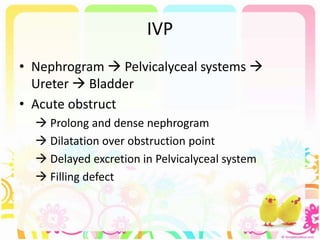
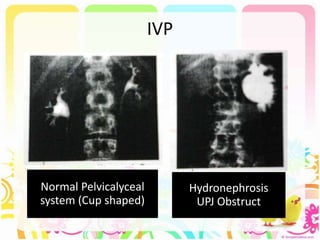
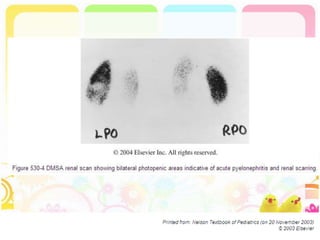
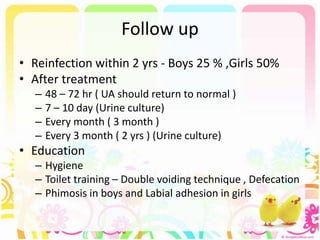
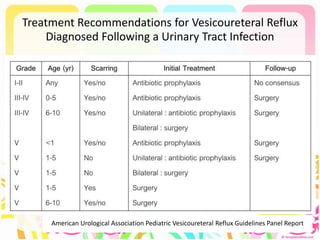
This case discusses a 13-year-old Thai boy presenting with right flank pain and urinary tract infection symptoms for 1 day. Physical examination found costovertebral angle tenderness on the right side. Investigations including urine analysis, urine culture and ultrasound were performed. He was diagnosed with acute urinary tract infection and treated with intravenous antibiotics. Follow up showed resolution of symptoms and no growth on repeat urine culture. Management included treatment of the acute infection and plans for prevention of recurrence through antibiotic prophylaxis and radiological investigation given his risk factors.