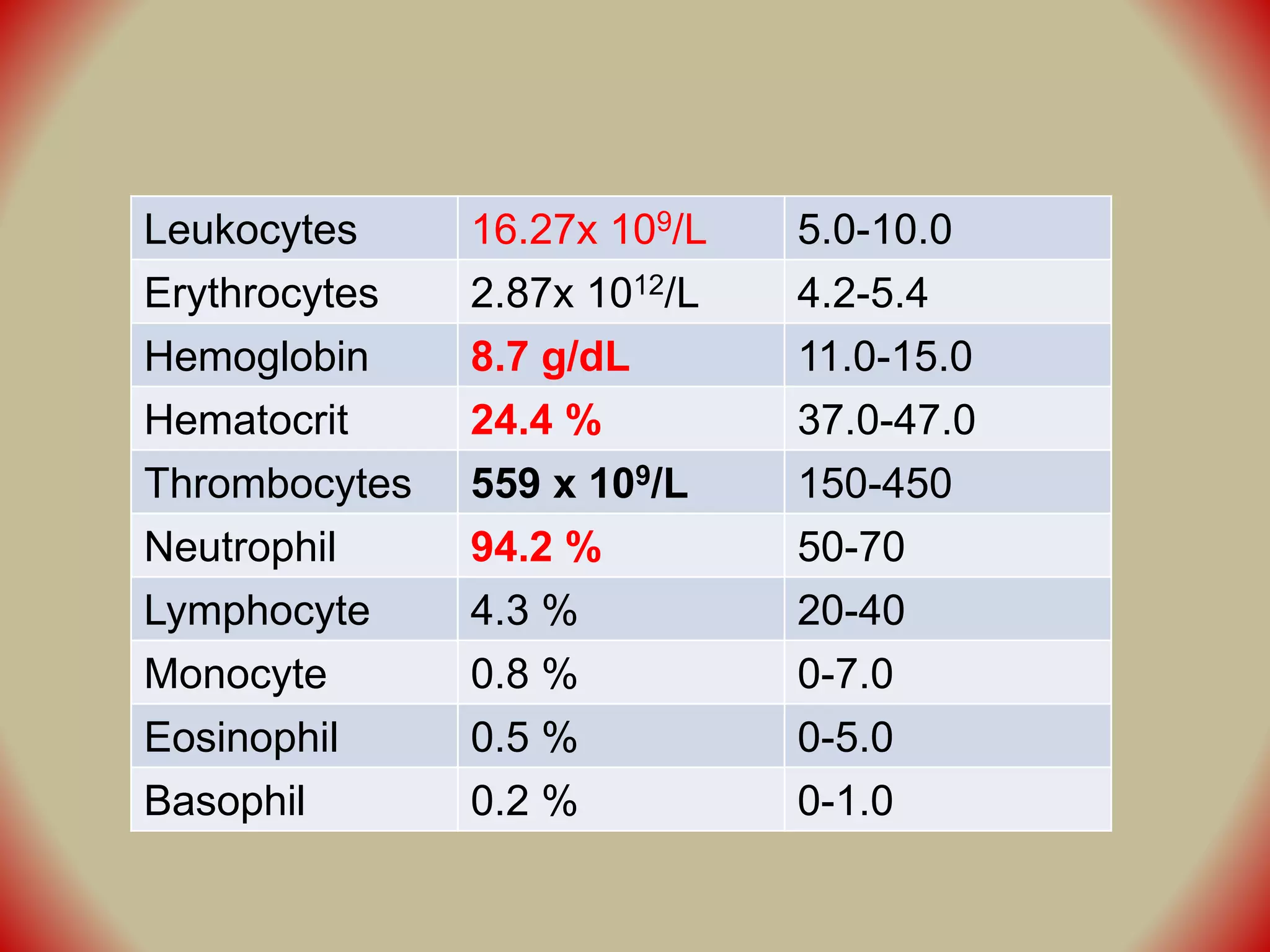
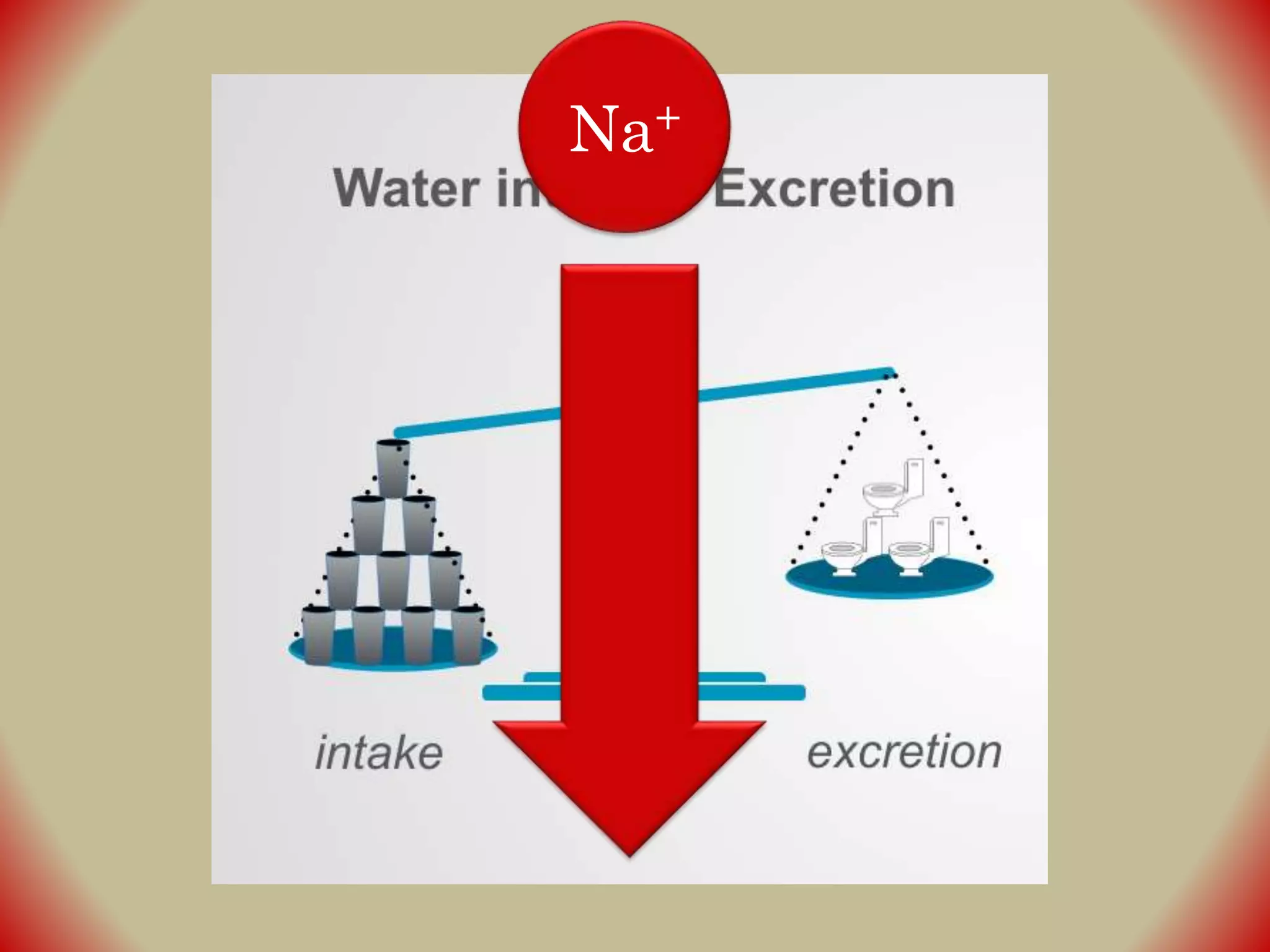
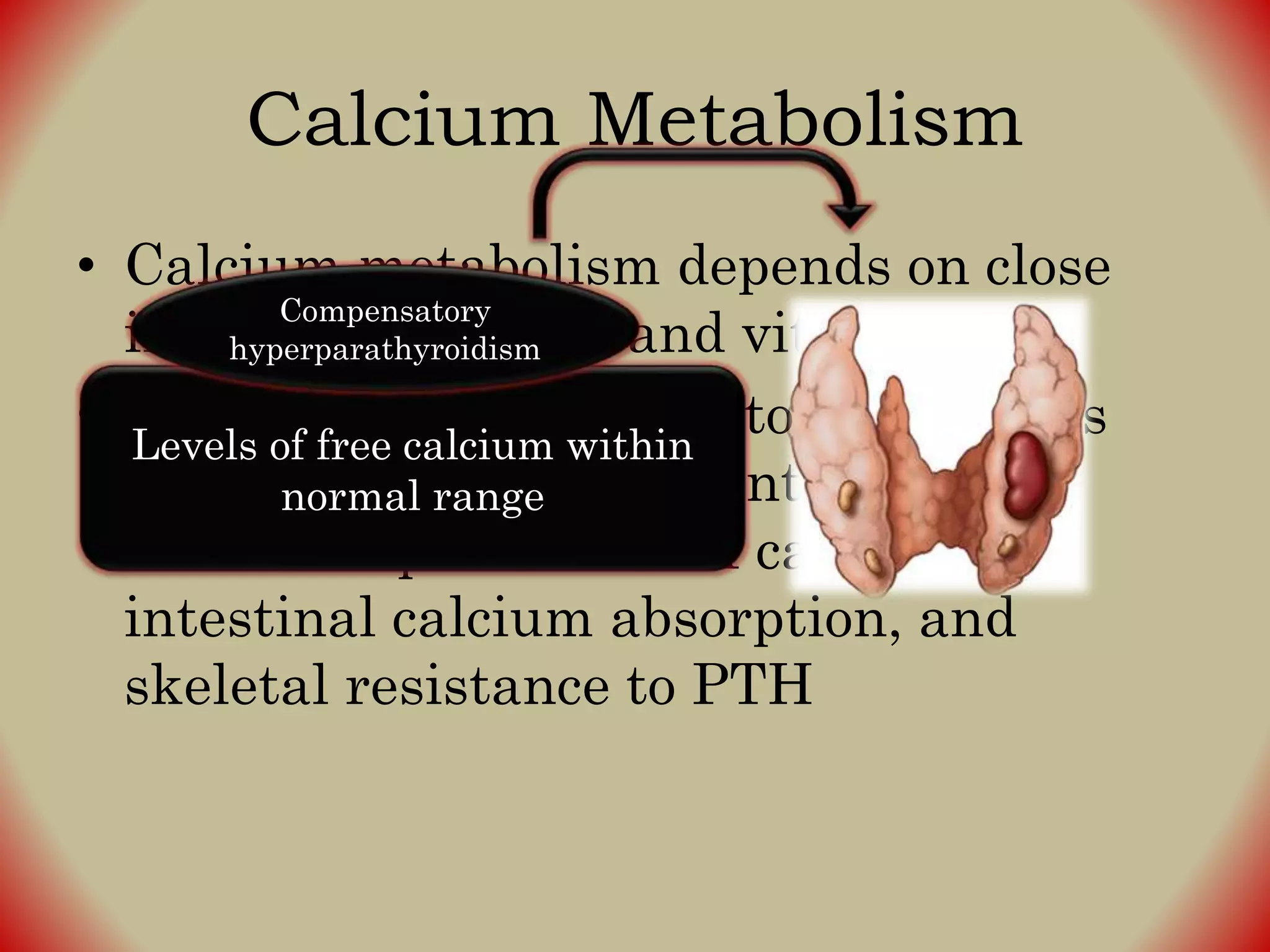
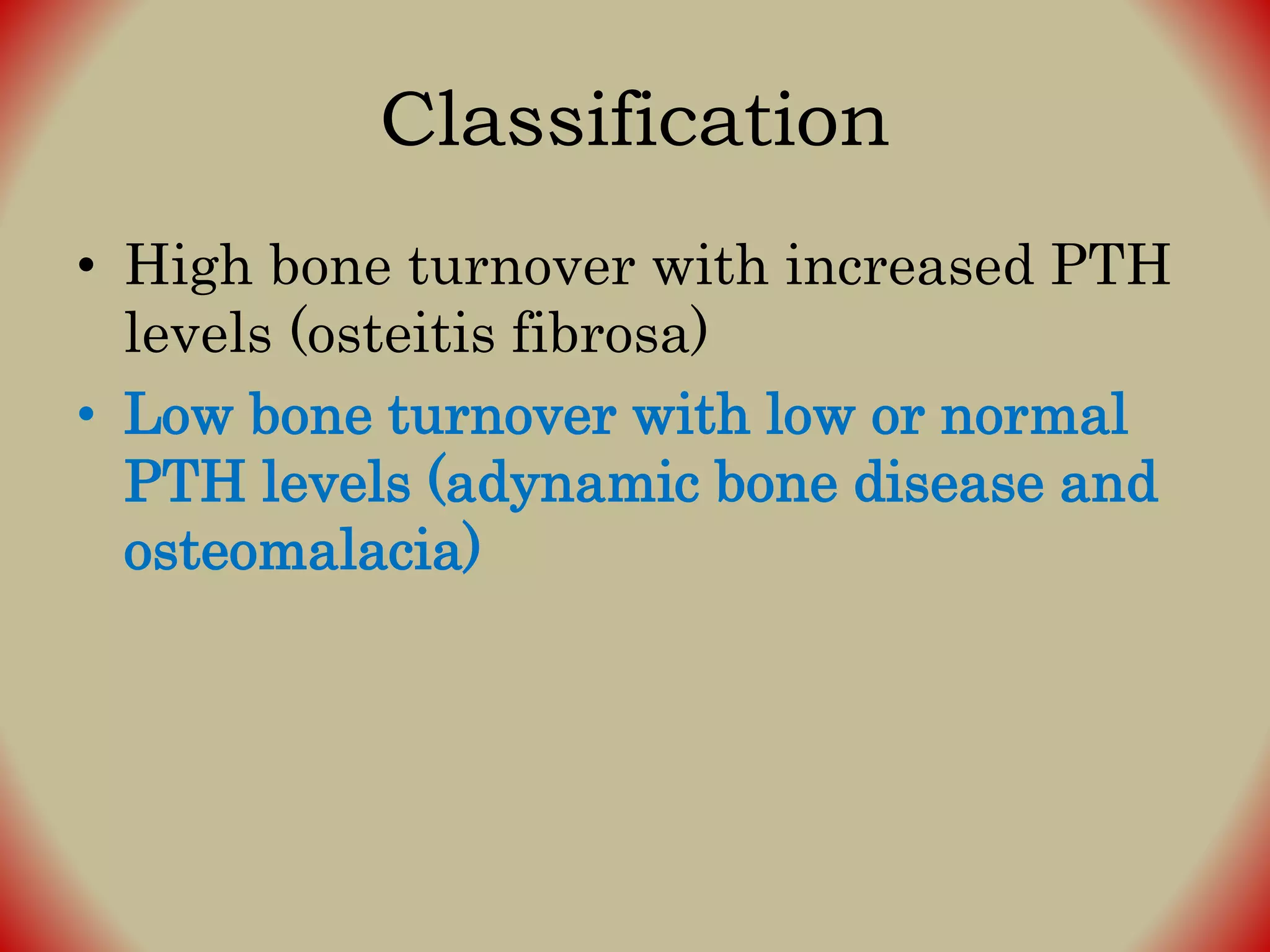
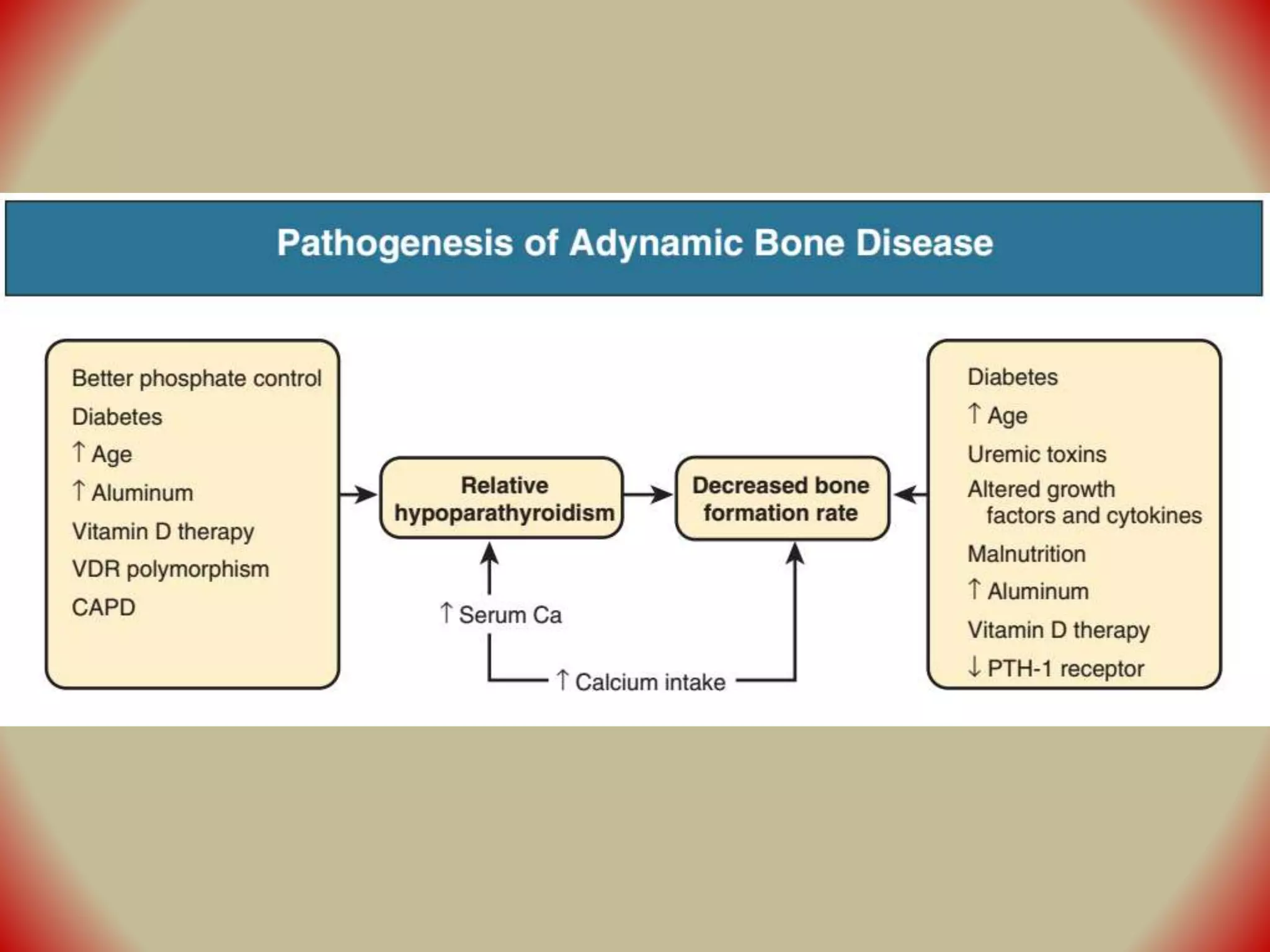
This document describes various complications that can arise in patients with end-stage renal disease (ESRD). It discusses difficulties regulating sodium, water, potassium and acid-base balance as kidney function declines. It also covers bone disease manifestations like osteitis fibrosa and adynamic bone disease. Treatment focuses on restricting dietary sodium/potassium and using binders/supplements to manage electrolytes and bone abnormalities. The document also notes anemia is common in later-stage CKD due to insufficient erythropoietin production.