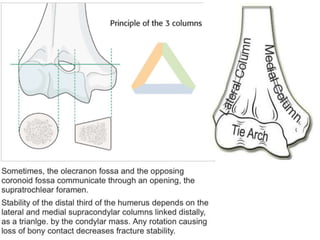
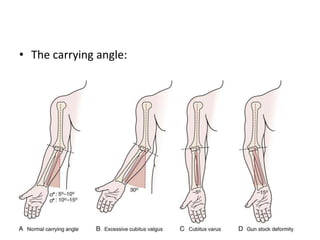
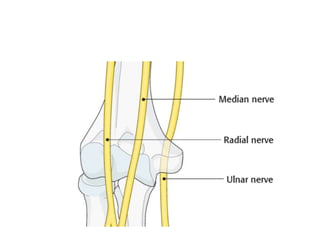
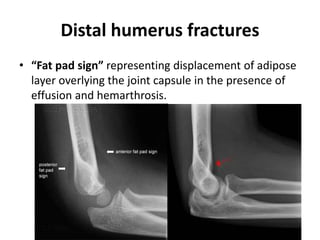
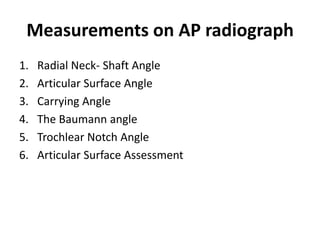
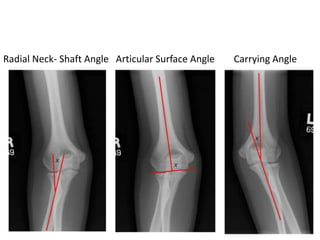
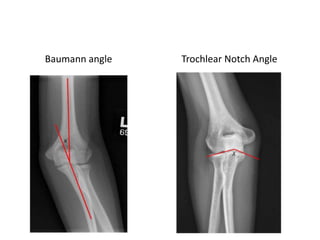
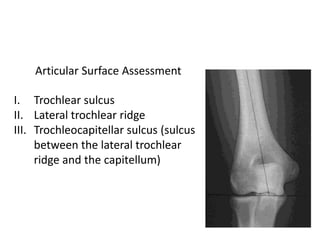
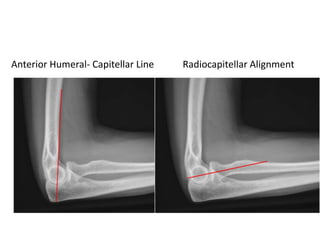
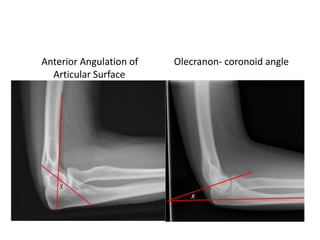
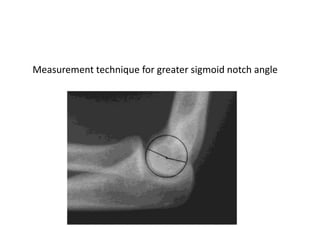
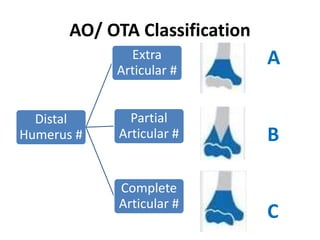
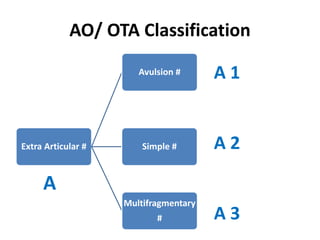
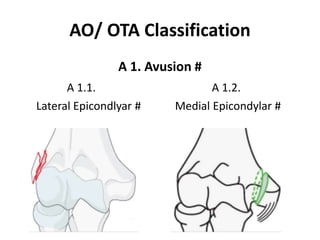
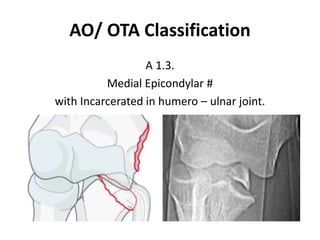
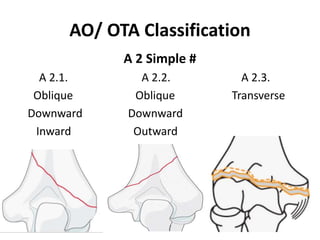
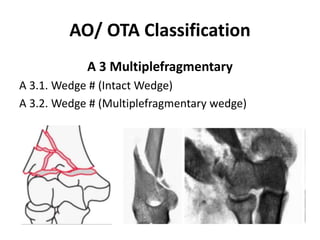
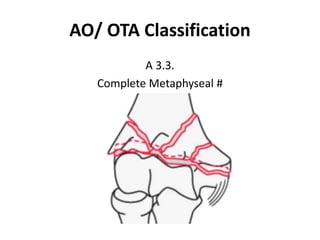
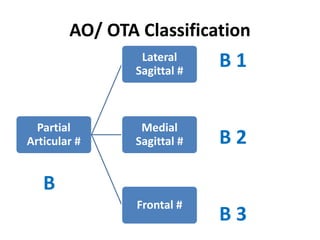
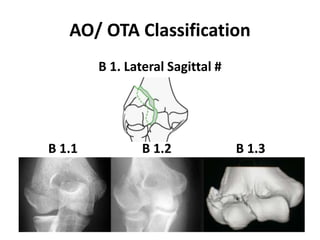
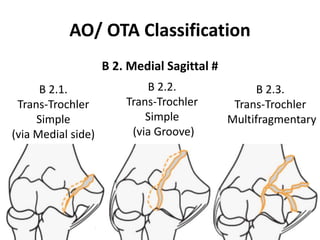
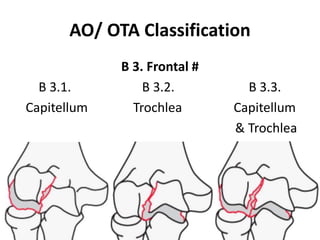
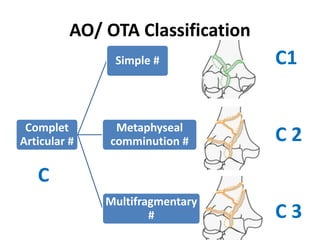
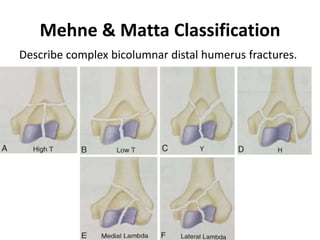
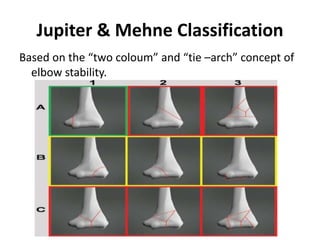
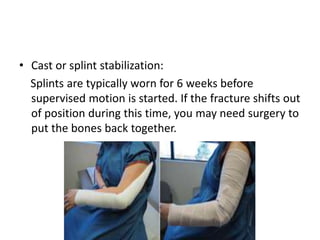
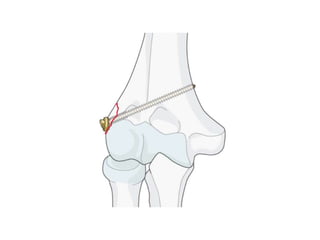
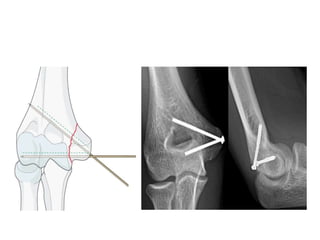
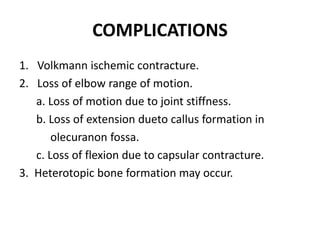
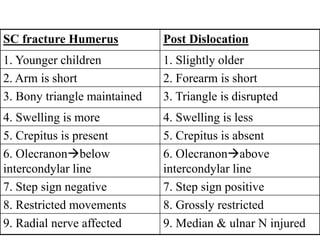
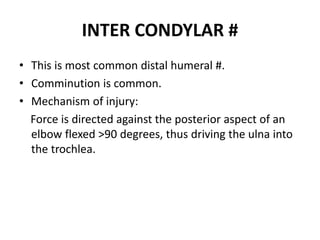
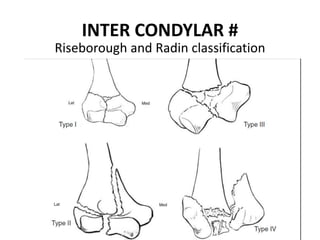
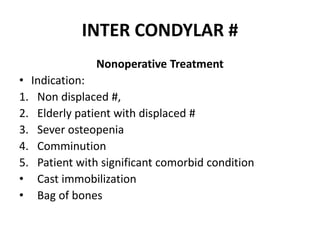
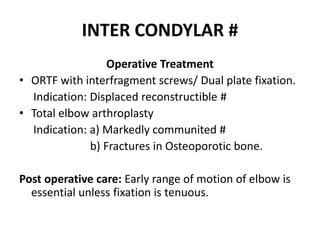
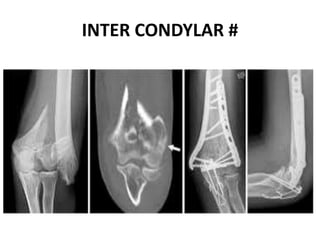
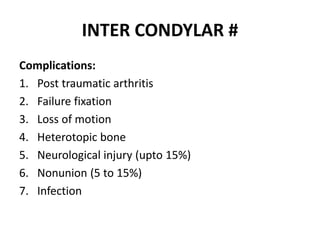
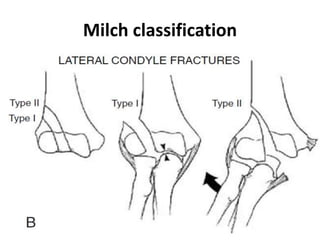
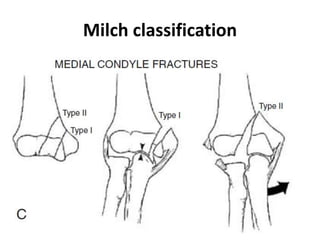
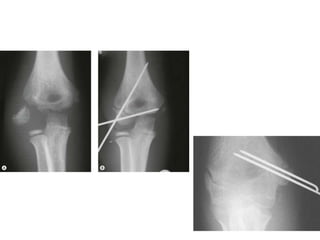
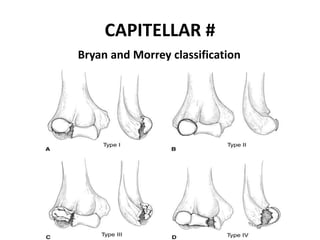
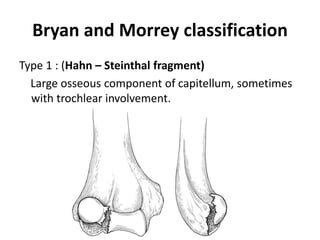
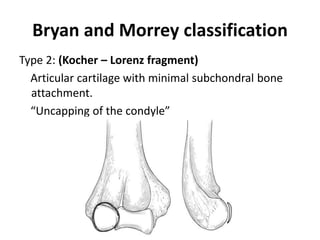
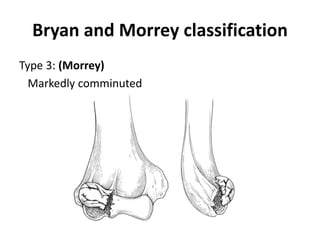
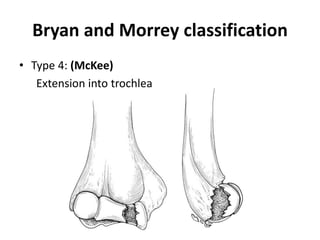
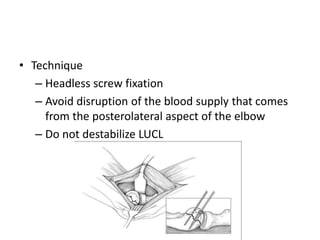
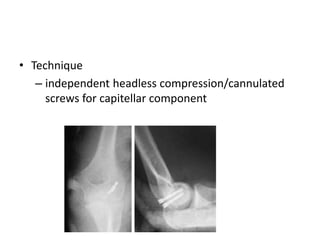
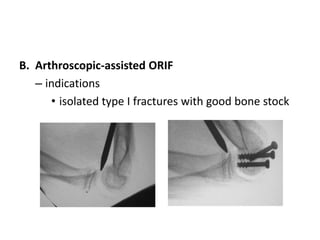
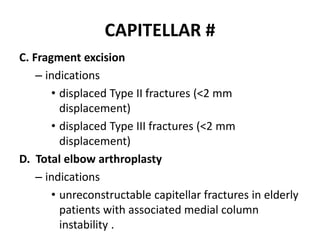
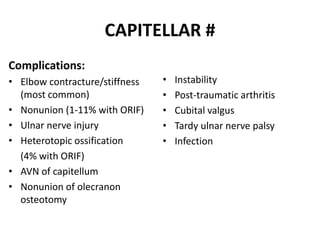
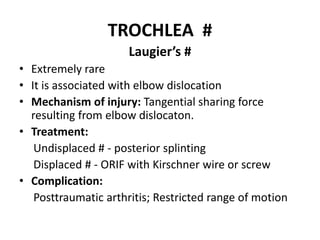
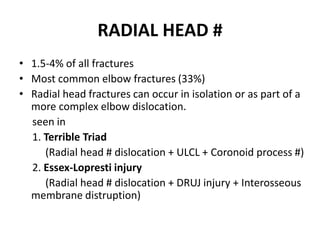
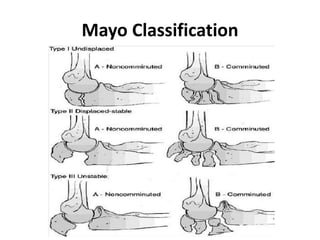
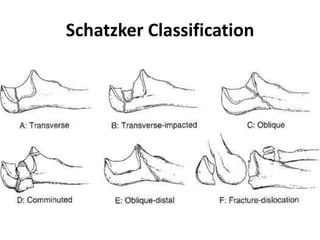
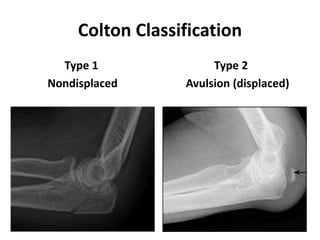
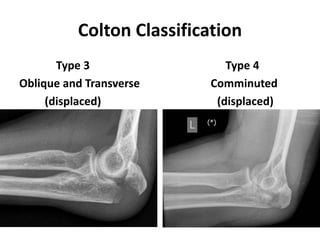
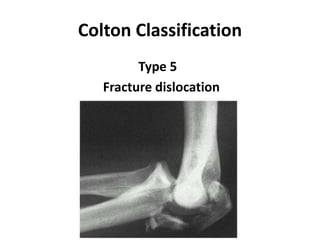
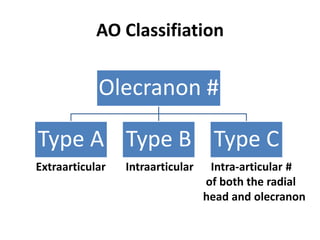
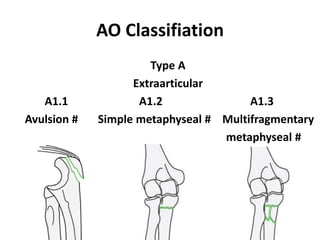
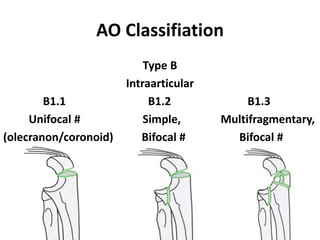
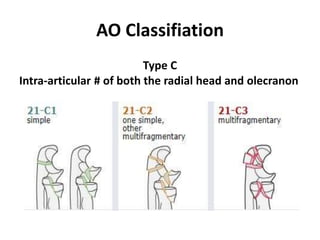
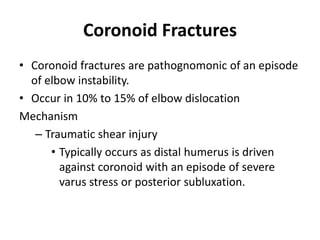
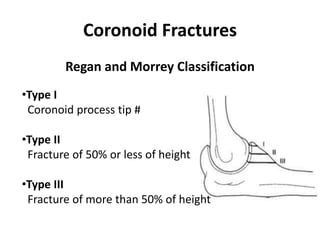
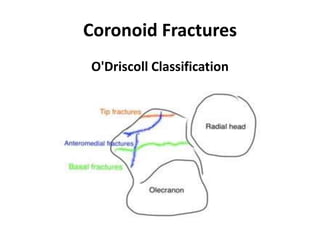
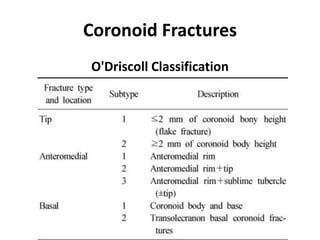
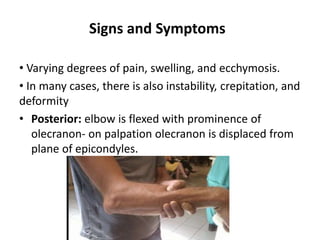
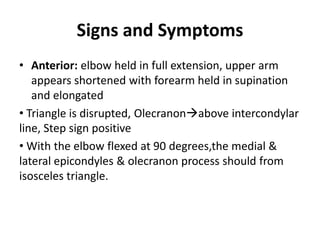
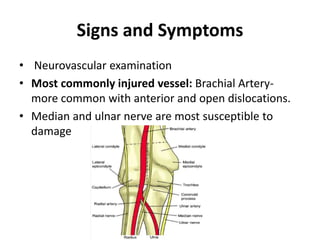
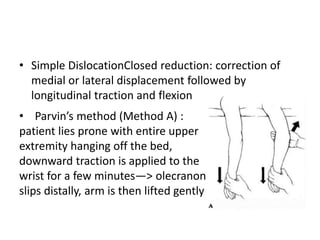
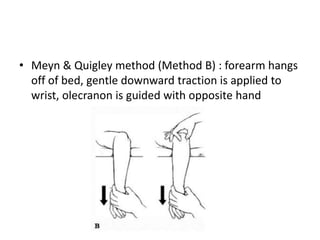
This document discusses various types of fractures of the distal humerus. It begins by describing distal humerus fractures in general, including common mechanisms of injury and clinical features. It then discusses specific fracture types - supracondylar, intercondylar, condylar, trochlear, and capitellar - providing details on classification systems, treatment options, and potential complications for each. Measurement techniques for radiographic evaluation and several classification systems used for distal humerus fractures are also summarized.