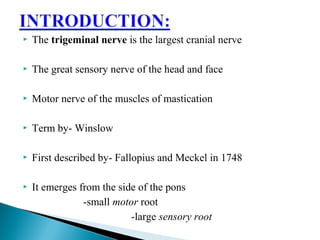
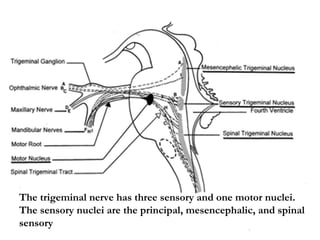
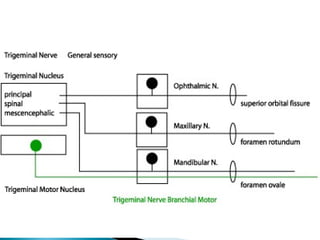
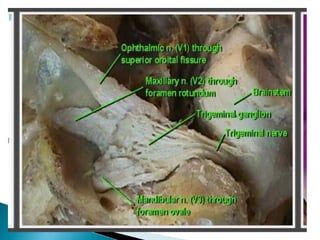
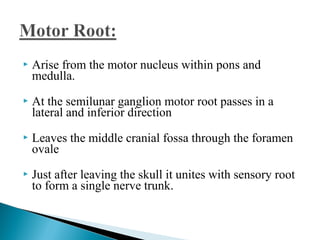
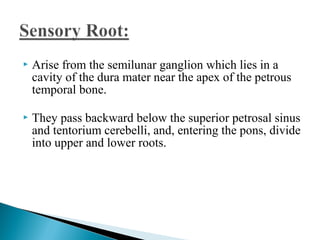
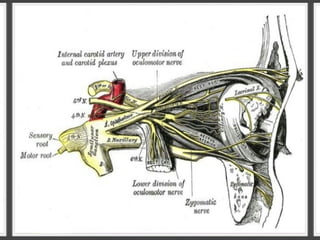
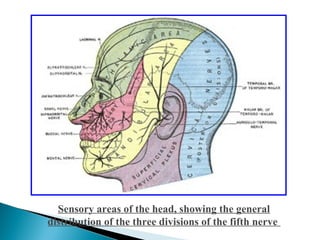
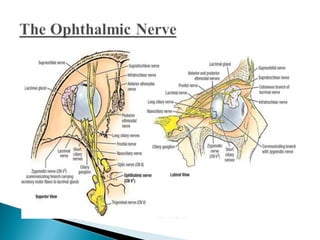
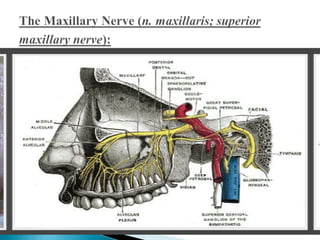
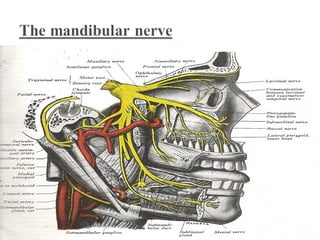
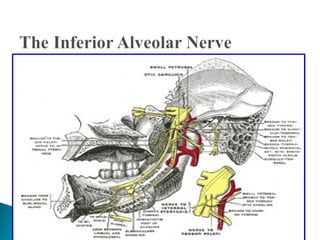
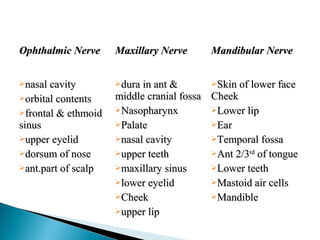
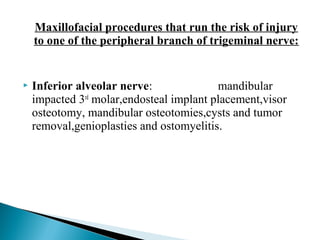
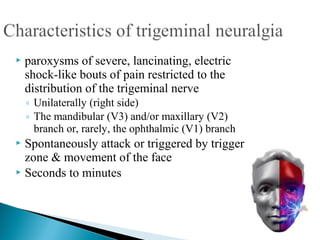
The trigeminal nerve is the largest of the cranial nerves. It has both sensory and motor functions, transmitting sensations from the face and motor commands to the muscles of mastication. The trigeminal nerve consists of three main divisions - the ophthalmic, maxillary, and mandibular nerves - which each have distinct sensory distributions and ganglia. Injuries or disorders of the trigeminal nerve can result in conditions like trigeminal neuralgia, which causes severe facial pain.