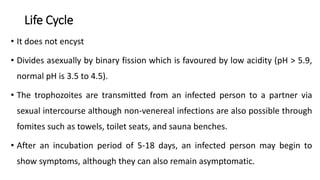
Trichomonas vaginalis is a protozoan parasite that causes the sexually transmitted infection trichomoniasis. It colonizes the lower genital tract of females or the urethra of males. The organism has no life stages other than the trophozoite form and divides asexually. Infection occurs through sexual contact and symptoms include abnormal discharge and irritation. Diagnosis involves microscopic examination of discharge or culture testing. Treatment involves oral antibiotics like metronidazole which provide a high cure rate. Prevention focuses on treating partners and reducing risky sexual behaviors.