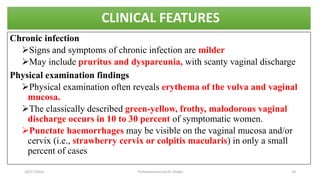
Trichomoniasis is a common sexually transmitted infection caused by the protozoan Trichomonas vaginalis. It primarily infects the urogenital tract of females and males. Symptoms can range from an acute inflammatory infection with symptoms like abnormal discharge to an asymptomatic infection. Diagnosis is made through nucleic acid amplification tests or visualizing the motile trichomonads on a wet mount sample. Treatment involves oral metronidazole or tinidazole to cure the infection. Prevention focuses on limiting sexual partners, condom use, and treatment of infected individuals to reduce transmission.