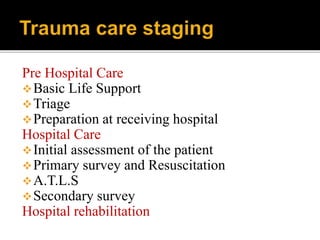
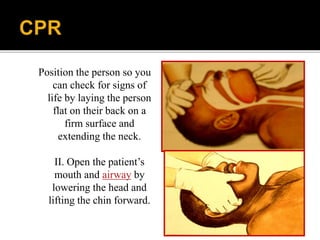
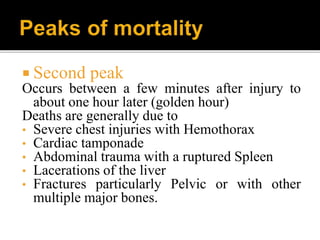
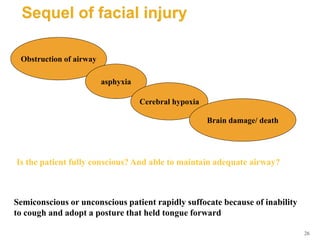
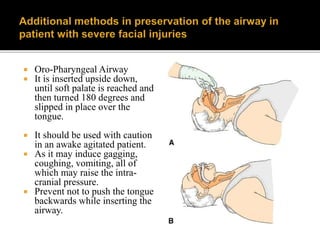
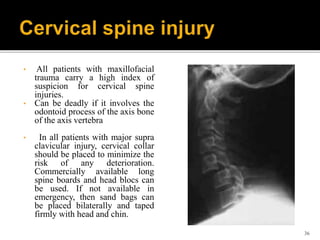
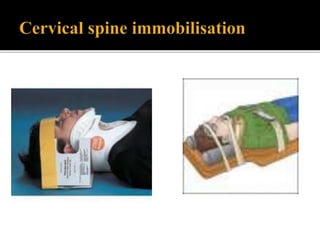
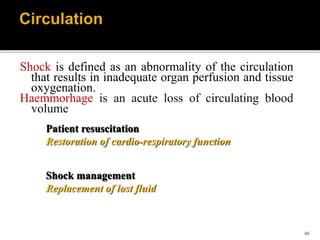
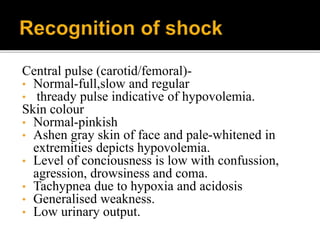
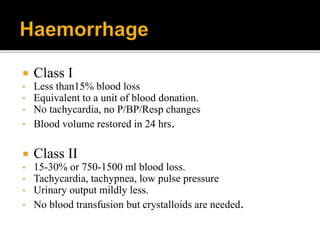
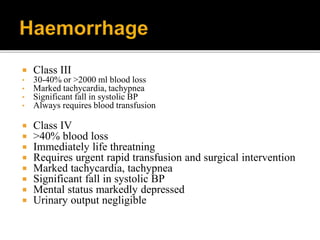
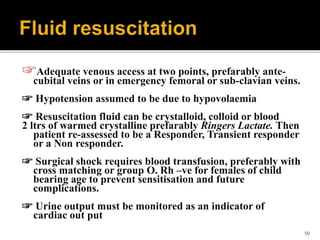
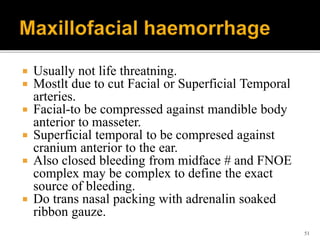
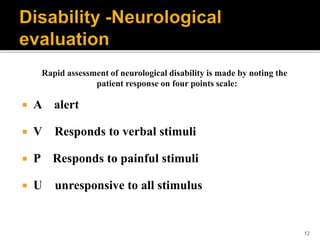
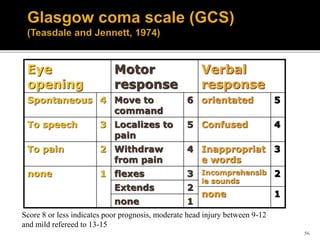
The document discusses trauma care and the "Golden Hour" concept. It emphasizes the importance of the first hour after injury, known as the Golden Hour, for trauma survival. It outlines the stages of trauma care from pre-hospital to hospital management, including basic life support, triage, ATLS protocols, and maximizing care during the platinum 10 minutes immediately following injury. Rapid assessment and stabilization of airway, breathing, circulation and disability are critical to survival.