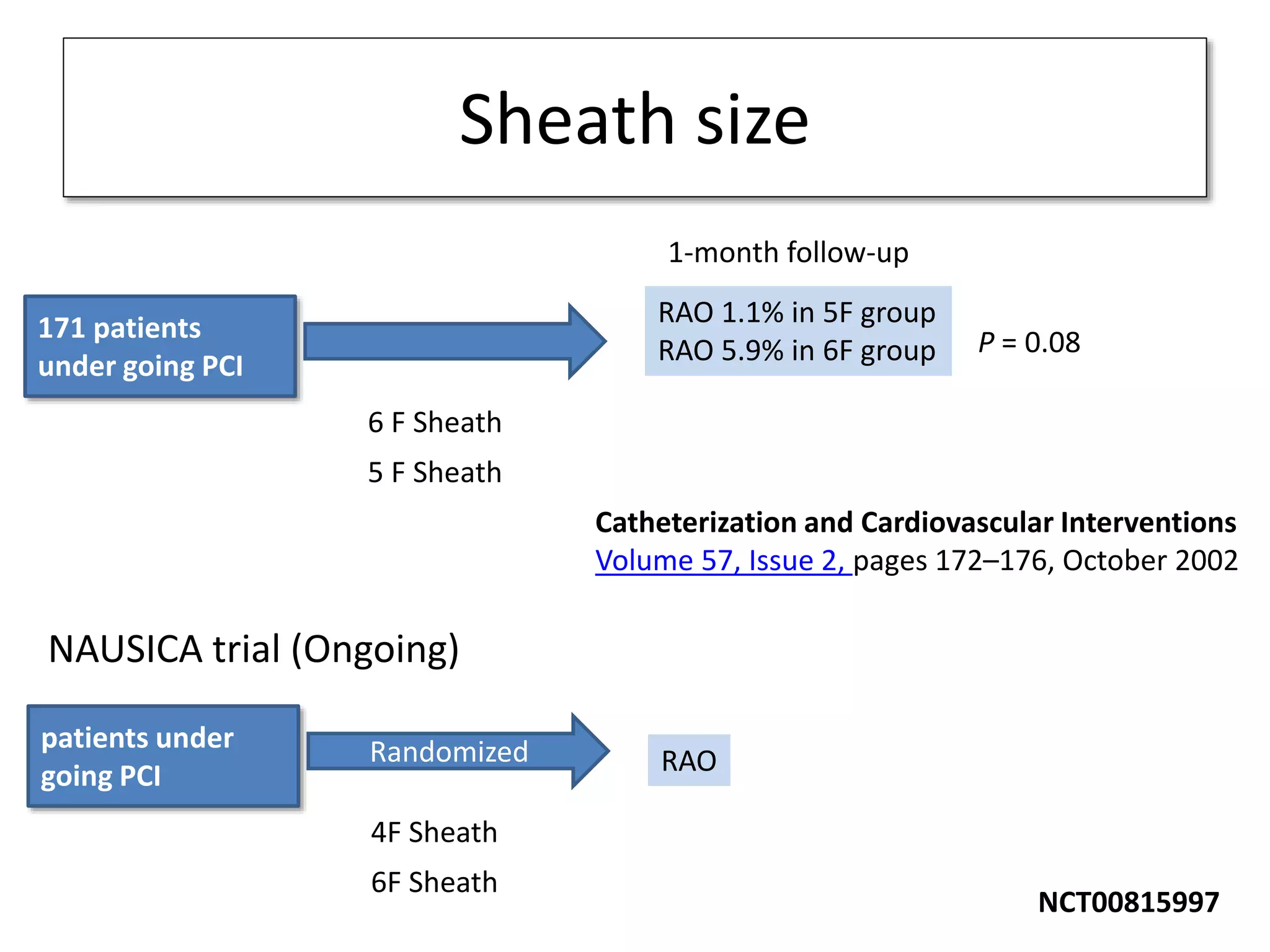
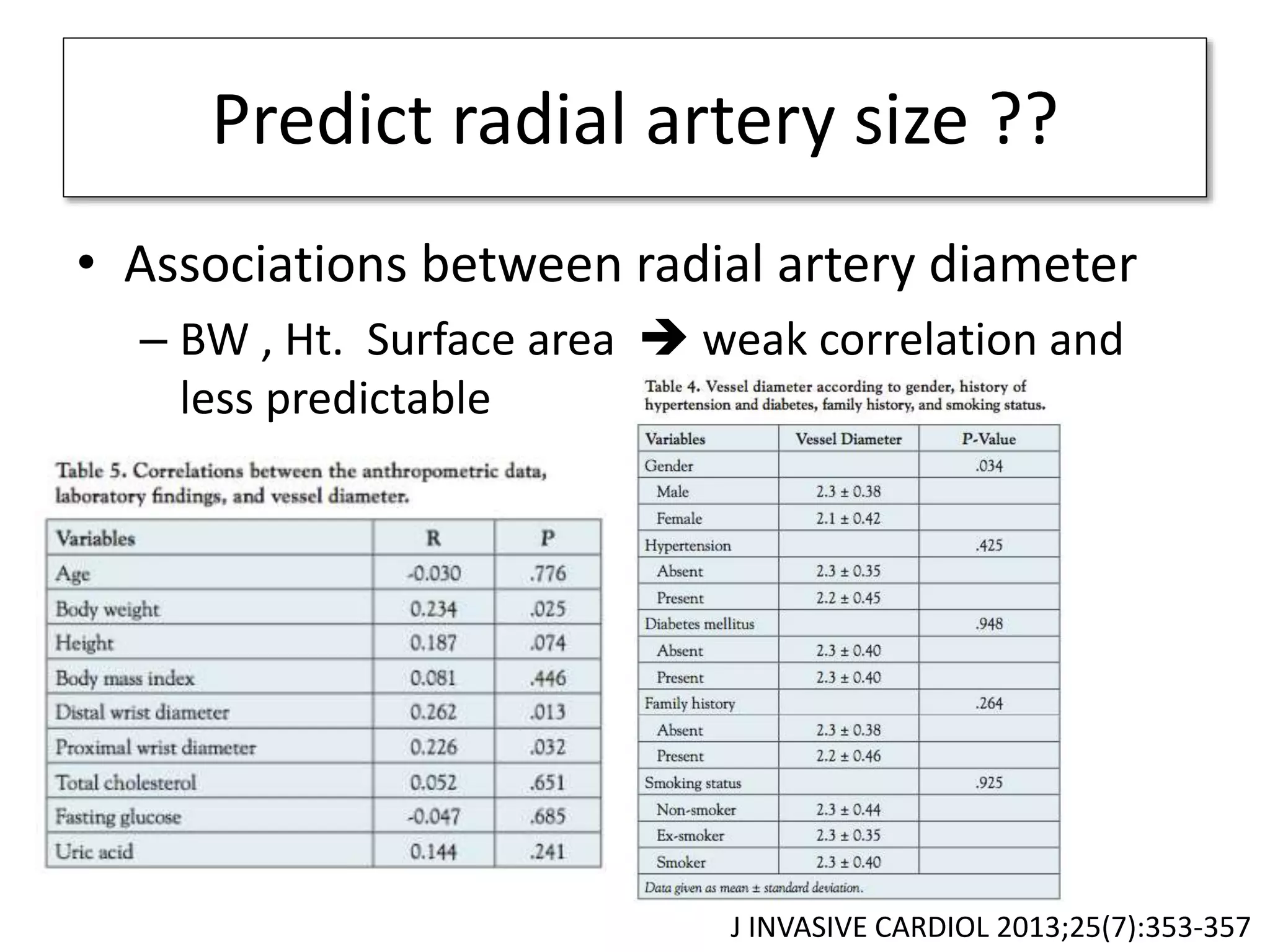
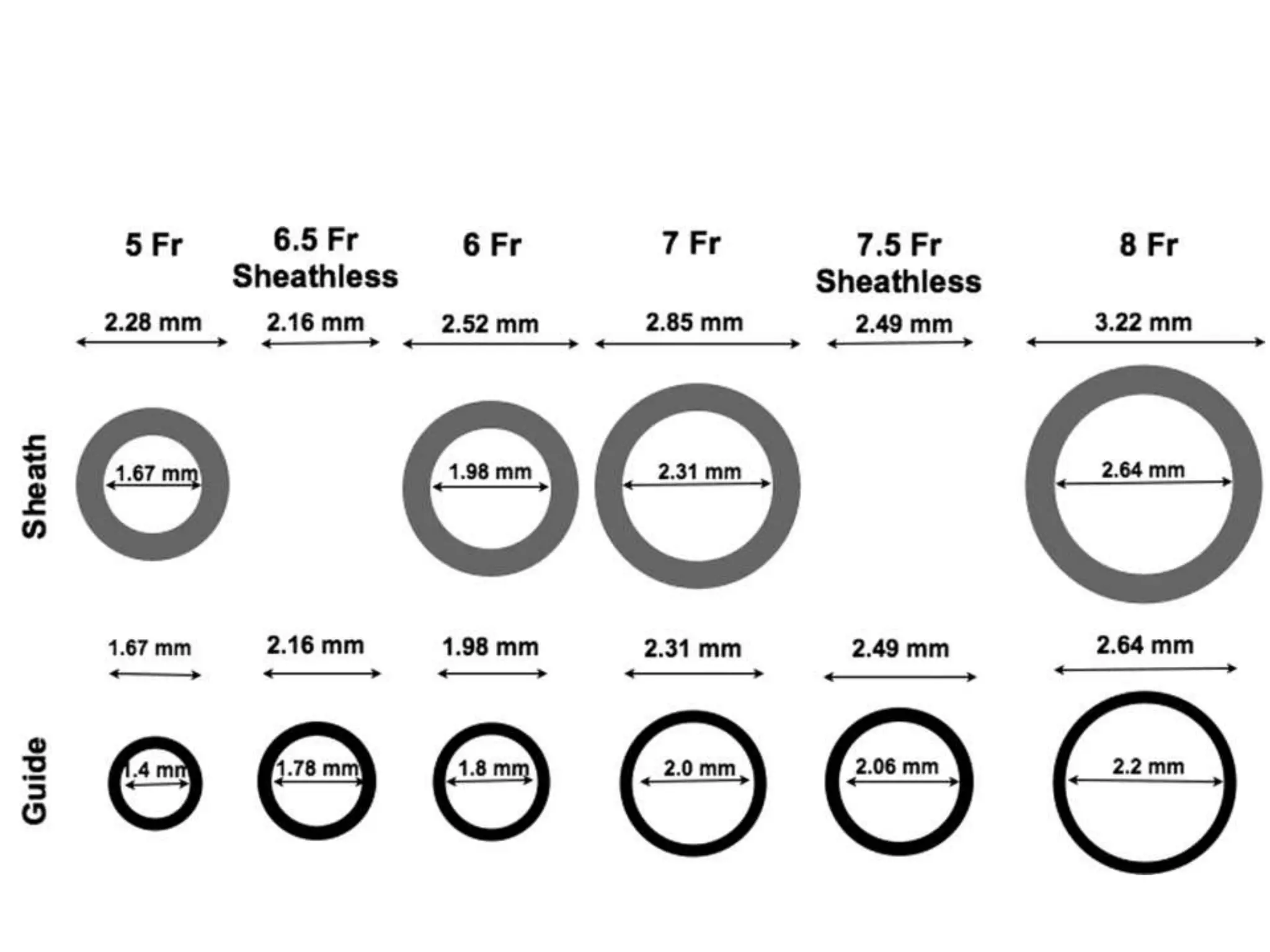
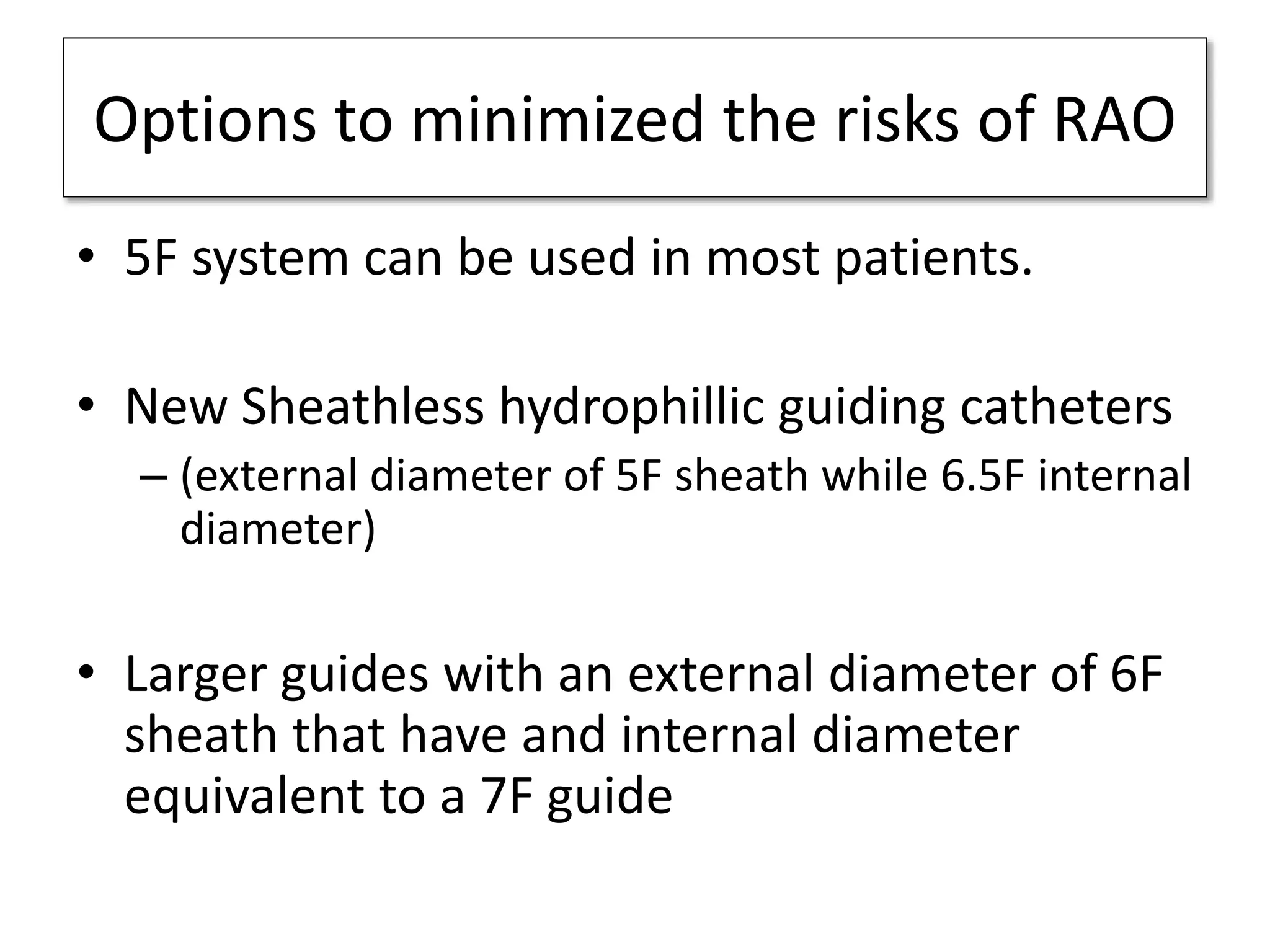
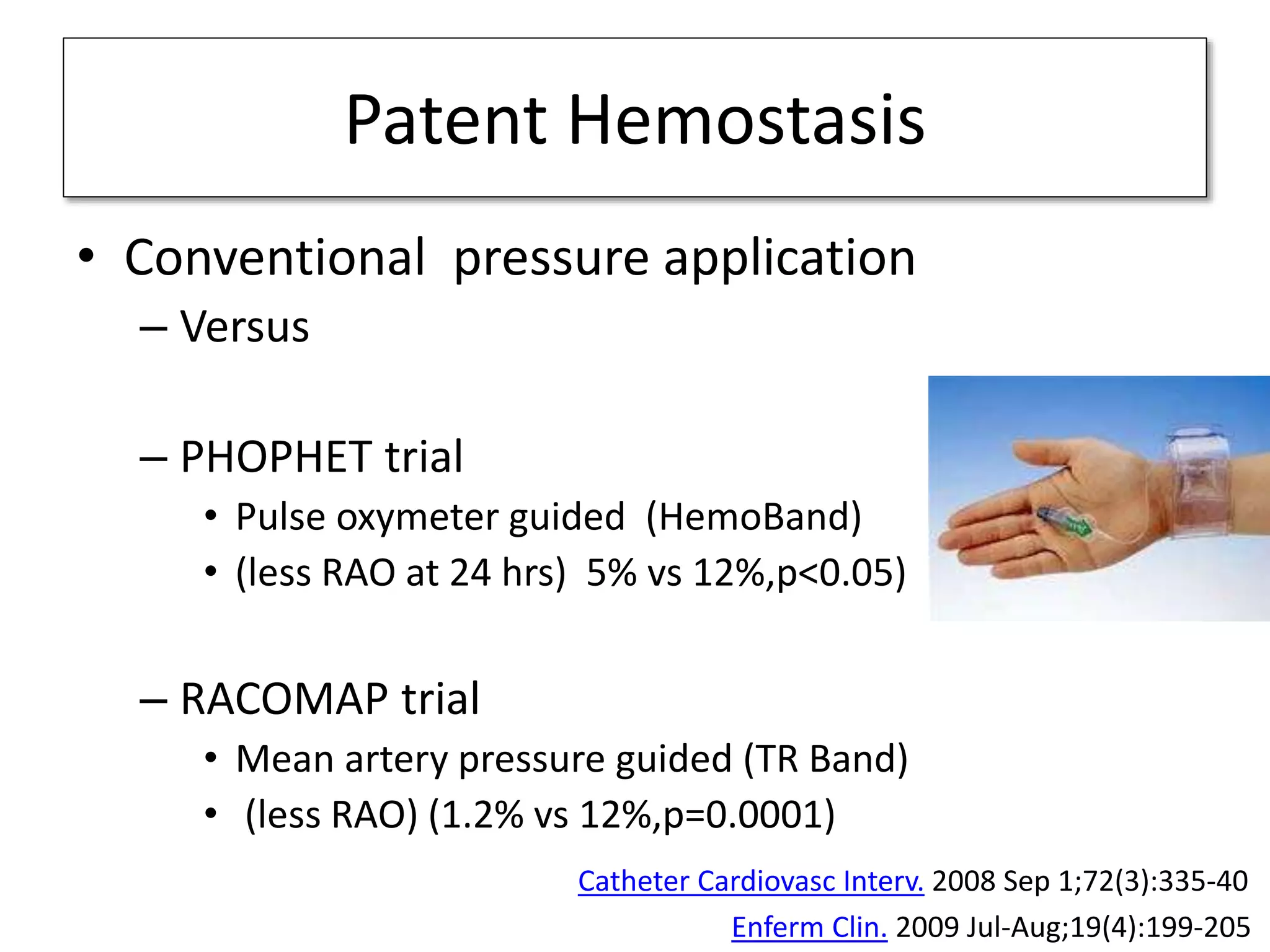
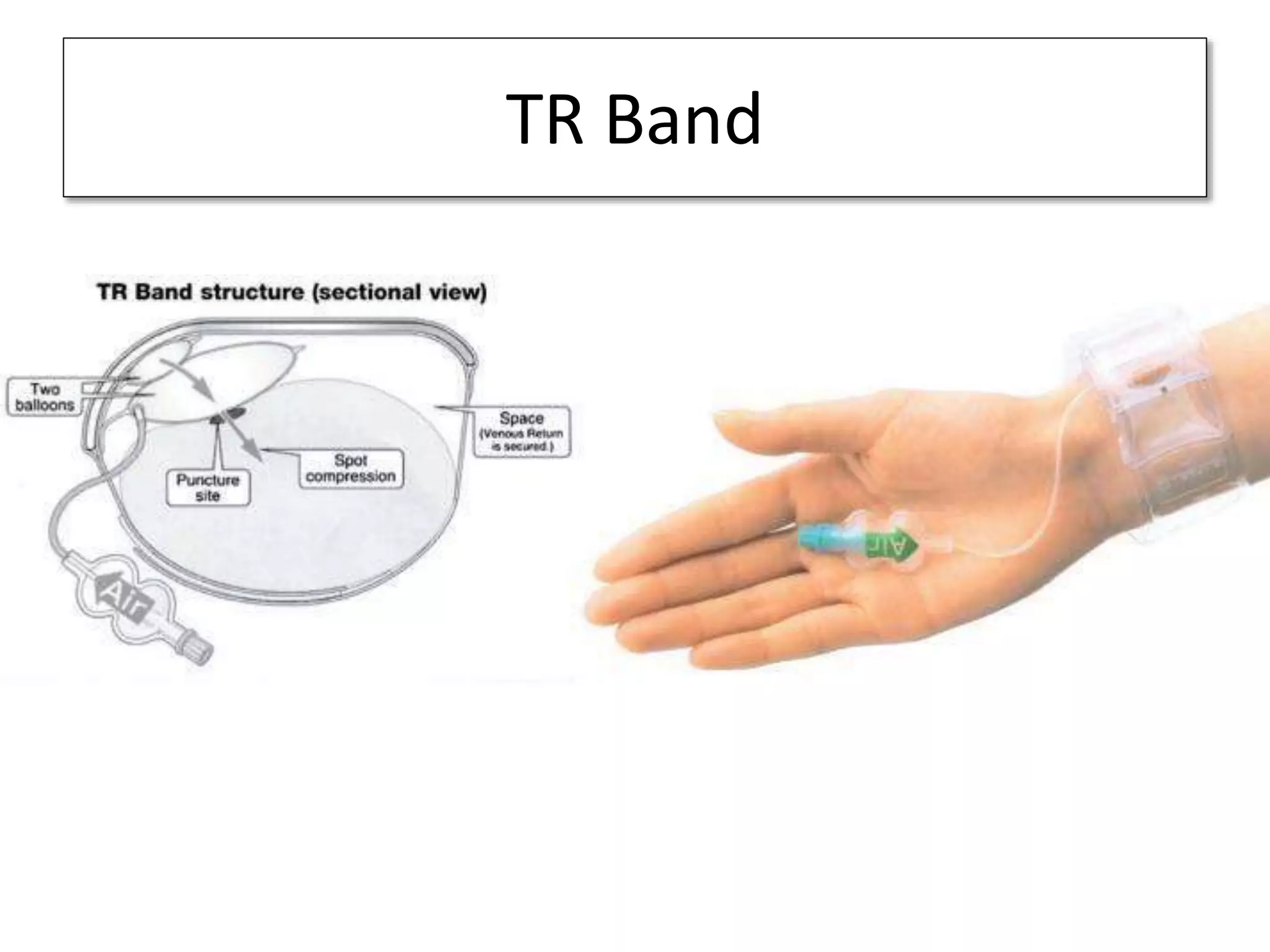
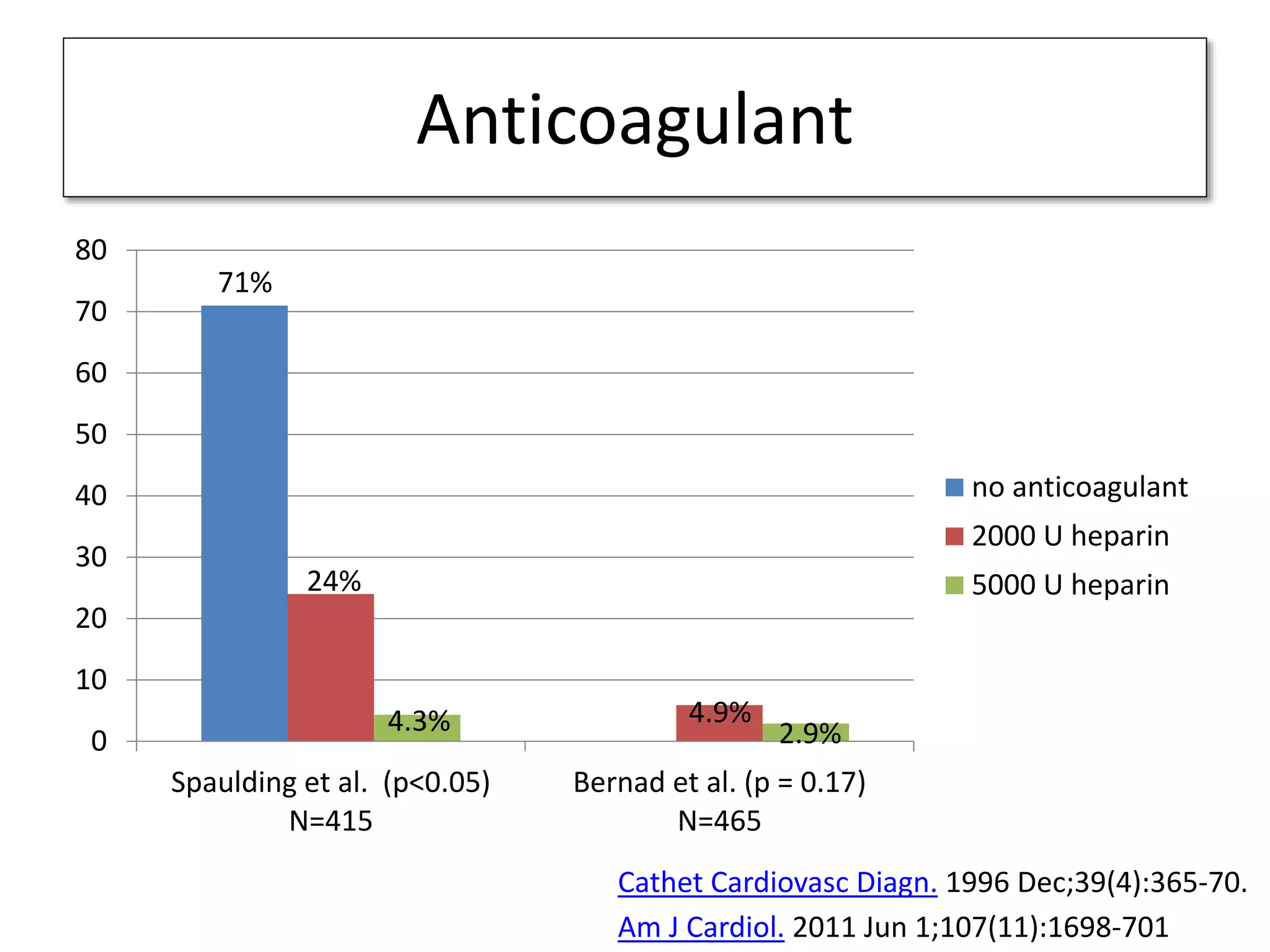
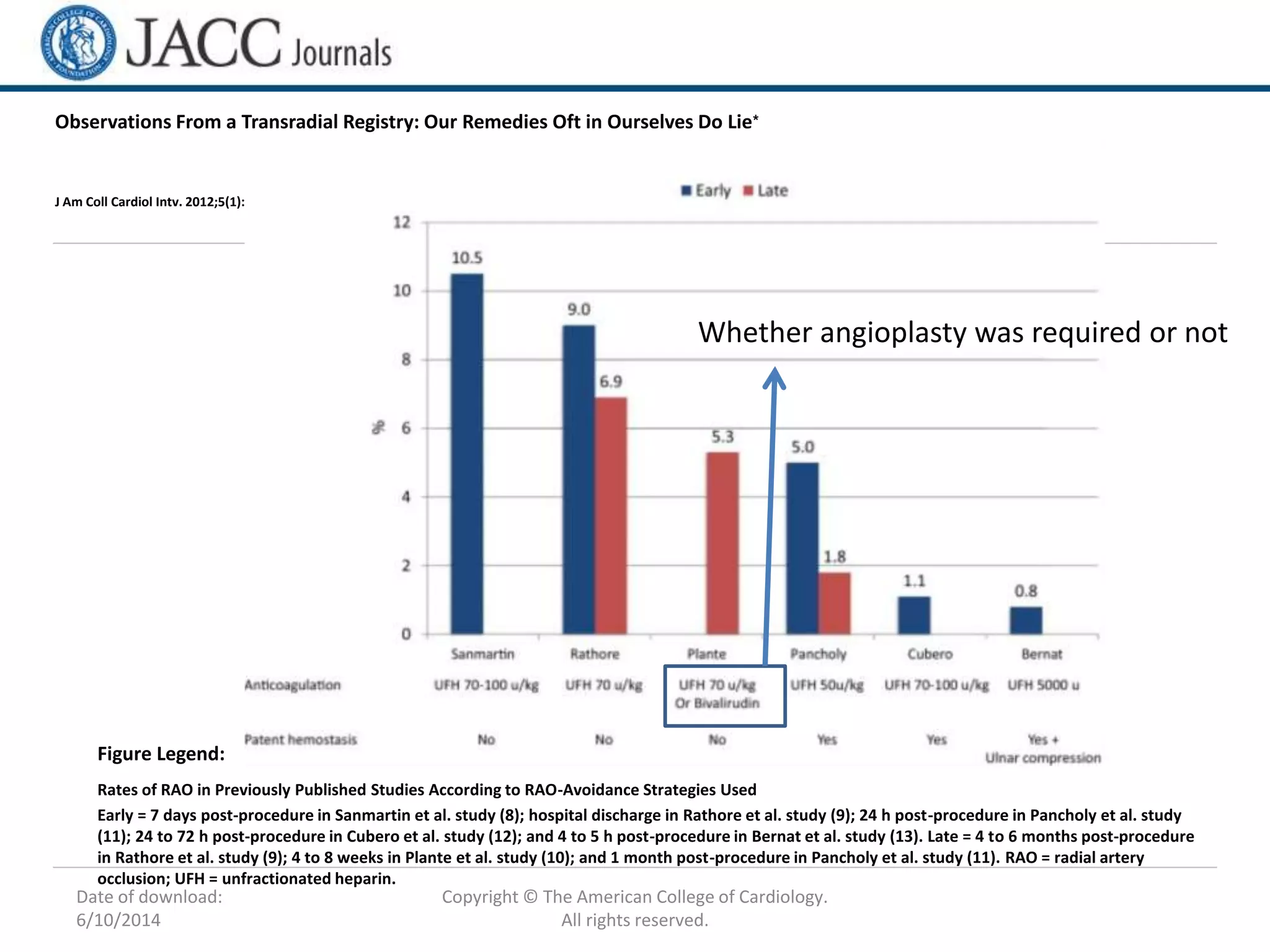
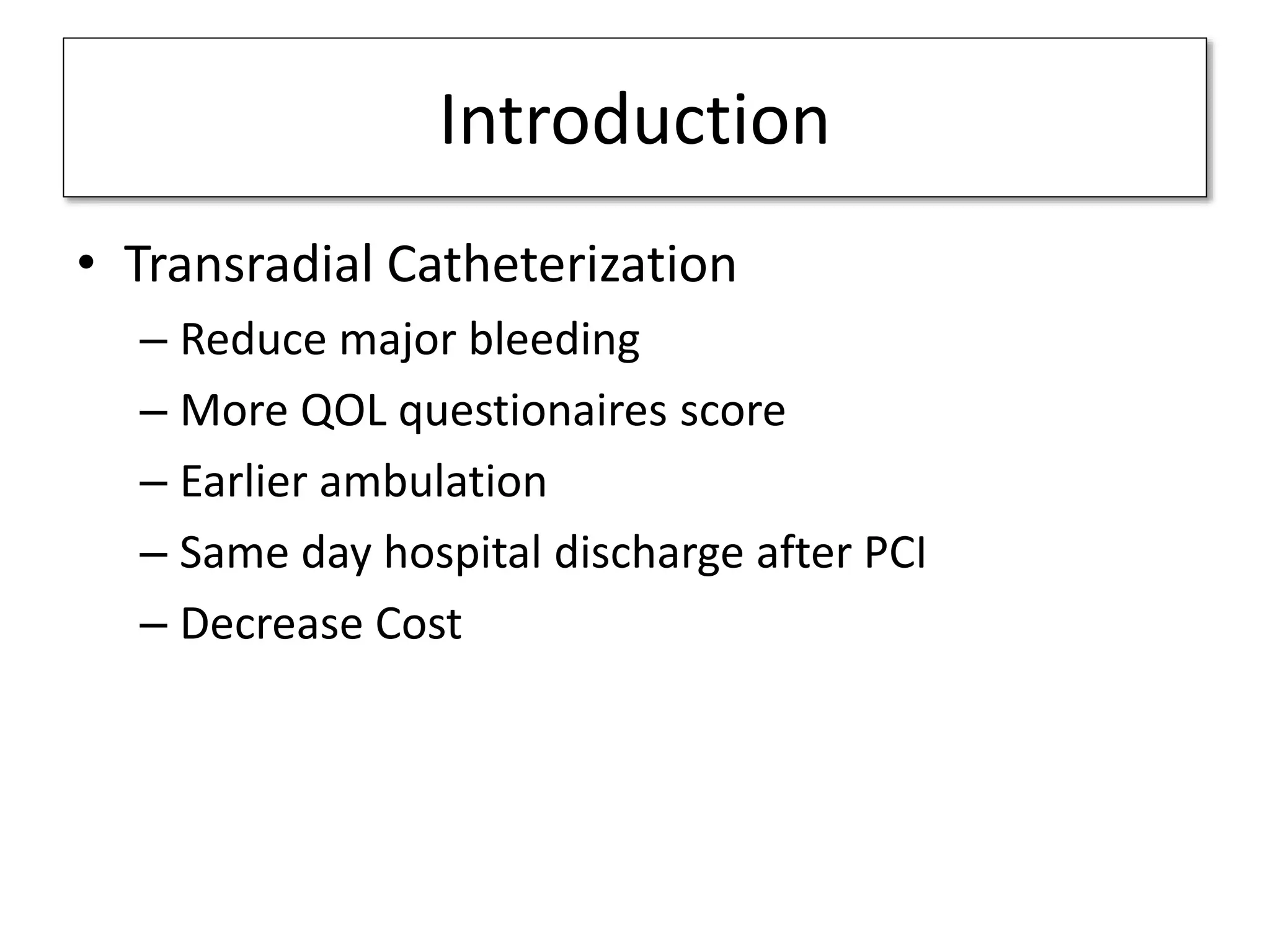
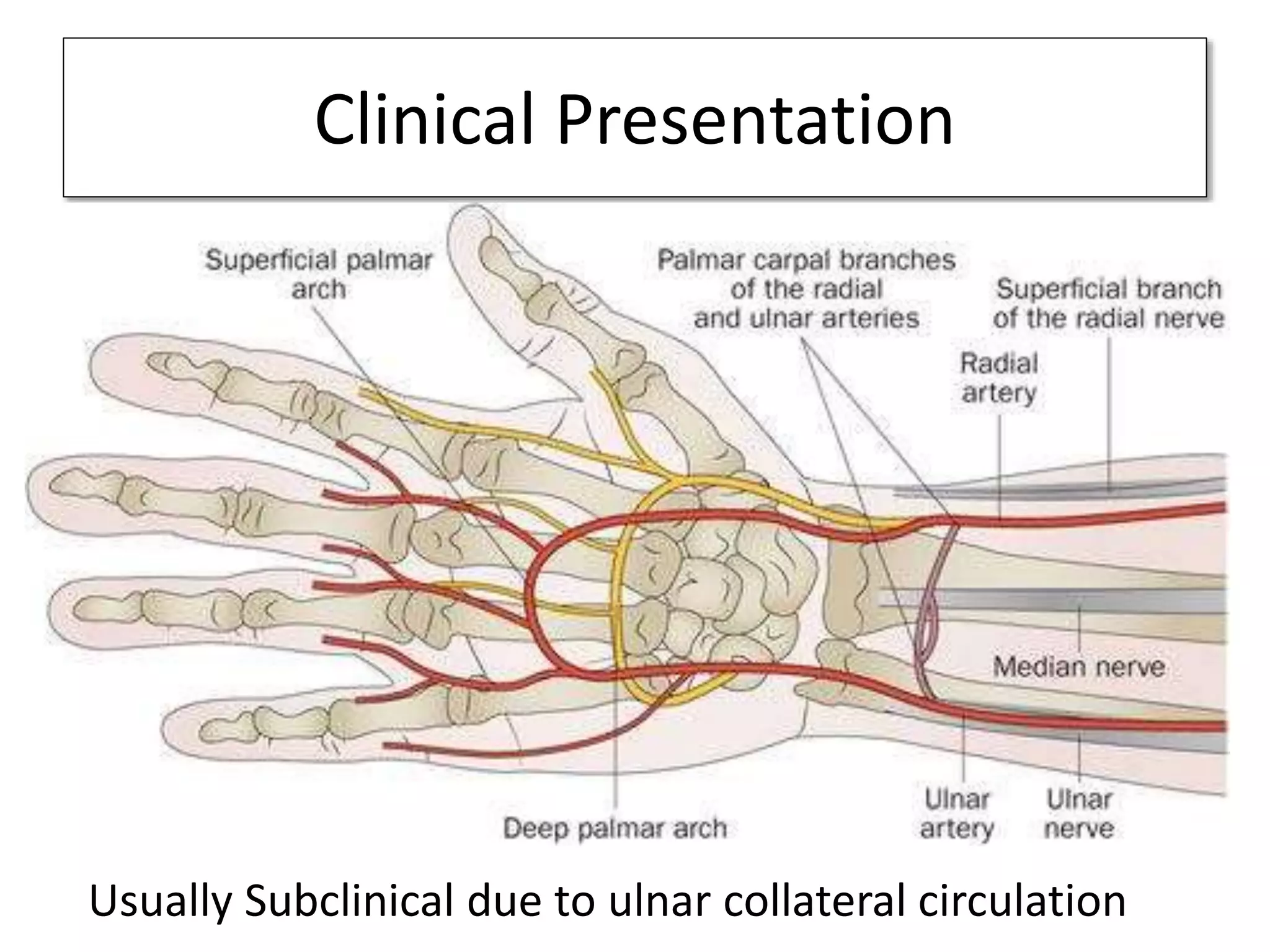
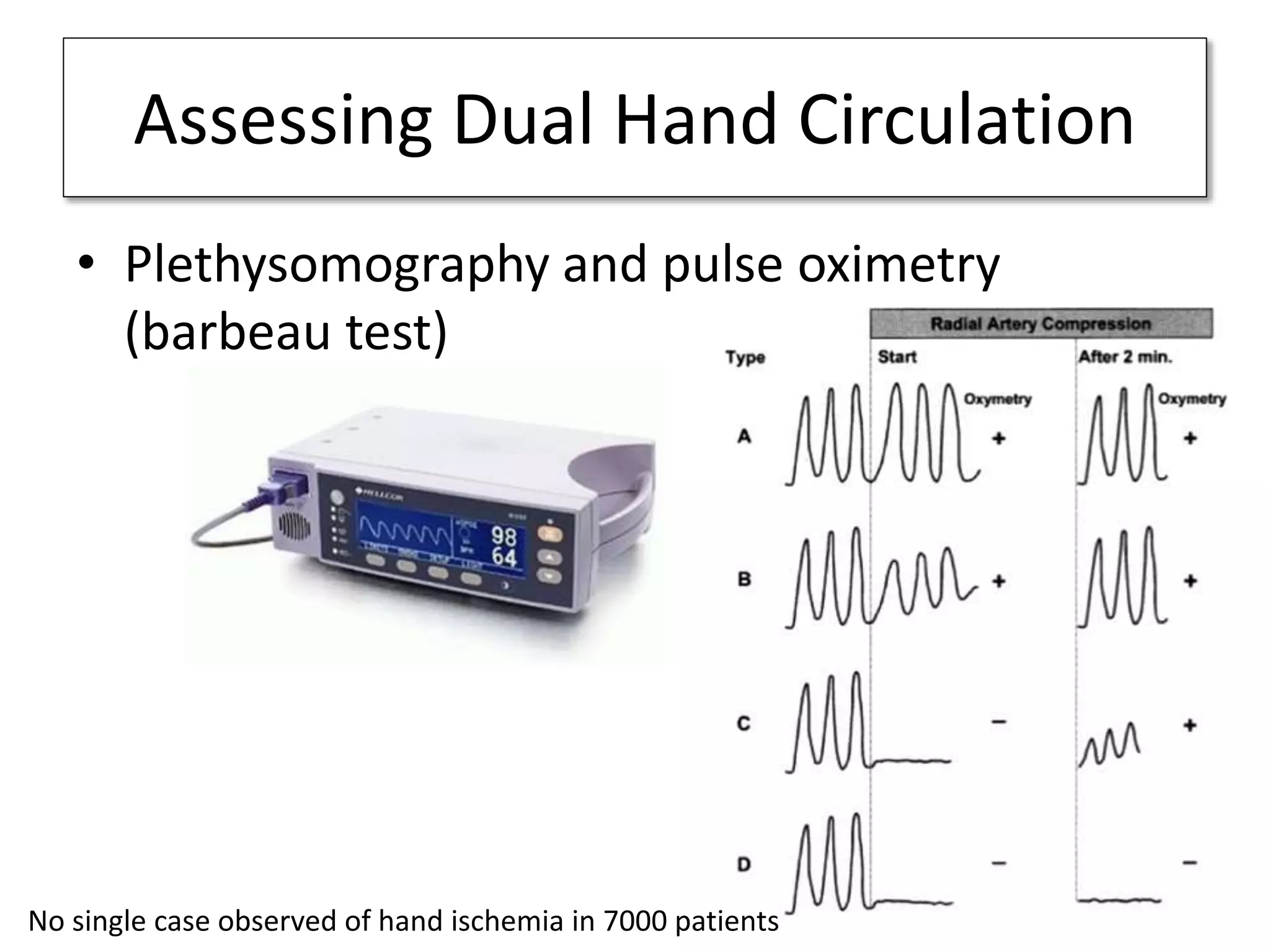
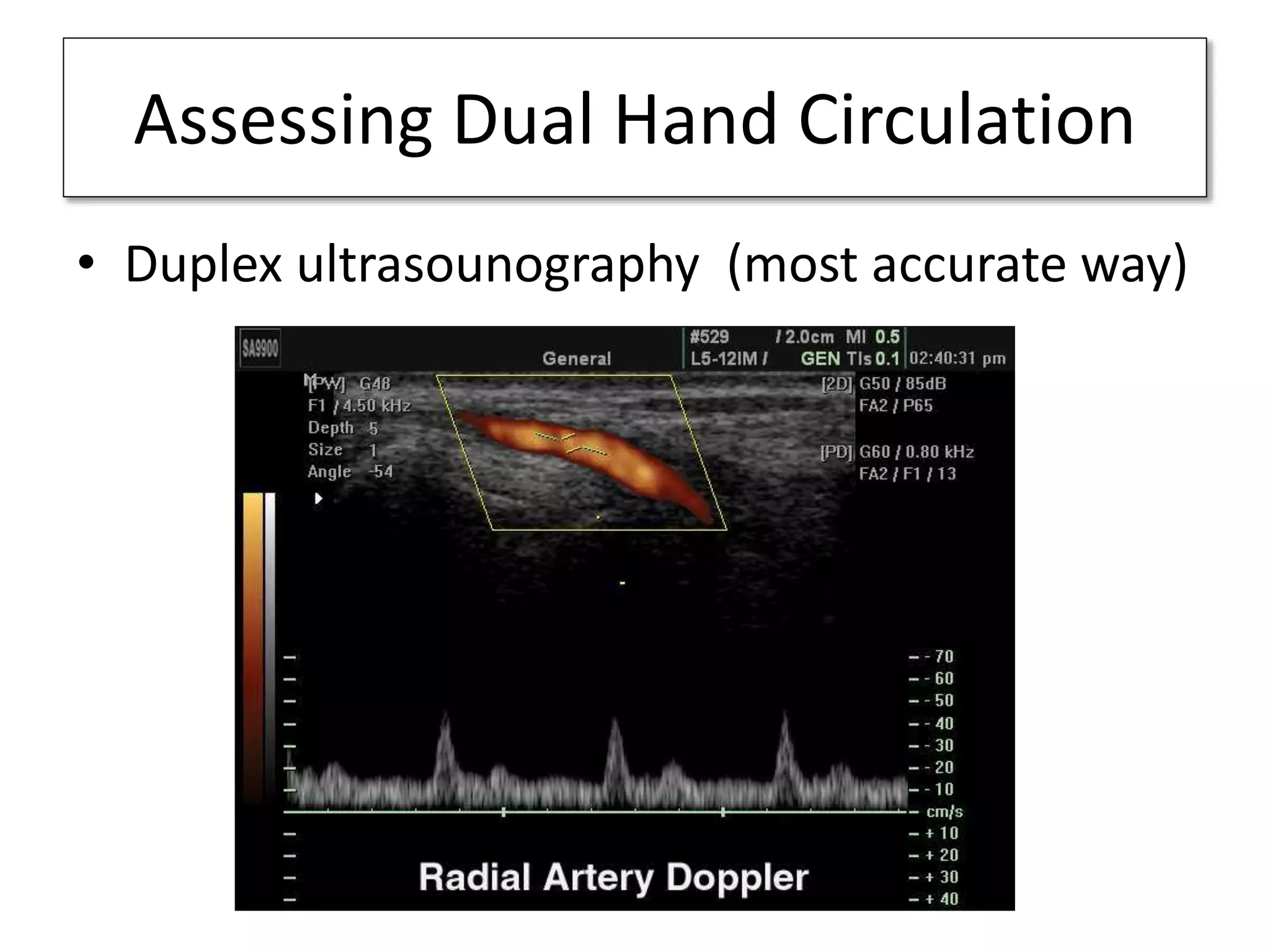
Radial artery occlusion can occur in 1-10% of cases after transradial catheterization due to thrombosis from endothelial injury after sheath insertion. While usually clinically silent due to dual blood supply, radial artery occlusion prevents future use of the artery for access. The risk of radial artery occlusion can be minimized by using smaller sheaths, avoiding excessive compression during hemostasis, and administering anticoagulants like heparin. Studies show pulse oximetry or pressure guided compression techniques and sheath sizes under 6 French reduce radial artery occlusion rates.

![Sheath size
• Oversized of Sheath
– vascular remodeling
– Thrombosis
250 patients
under going PCI
Pretreated
with NO
Journal of the Society for Cardiac Angiography & Interventions [1999, 46(2):173-178]
6F or larger inserted
S-A ratio > 1 RAO 13%
S-A ratio < 1 RAO 4%
(P=0.01)](https://image.slidesharecdn.com/radialarterypatencyaftertransradialcatheterization-140616084653-phpapp01/75/Radial-artery-patency-after-transradial-catheterization-20-2048.jpg)