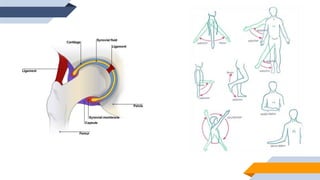
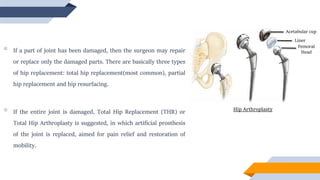
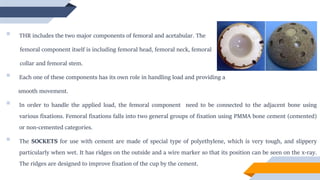
The document discusses total hip replacement surgery. It begins by describing hip anatomy and the components of a normal hip joint. It then explains the reasons why total hip replacement surgery becomes necessary, such as arthritis or injury. It provides details about the surgical procedure, including the different types of implants used to replace damaged bone and cartilage. The document discusses the history of hip replacement surgery and improvements in materials and techniques over time. It concludes by noting possible complications after surgery, such as blood clots, infection, or implant loosening over years.