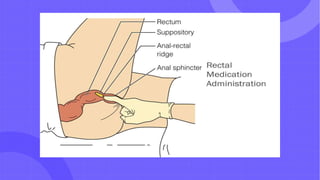
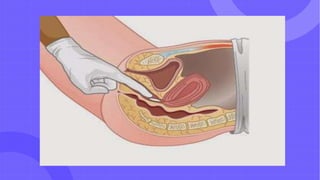
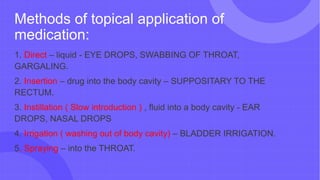
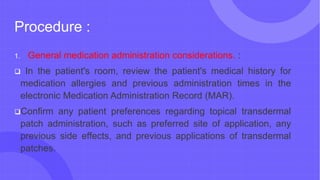
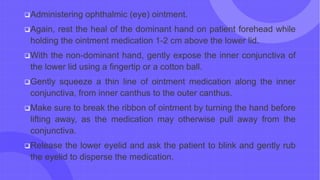
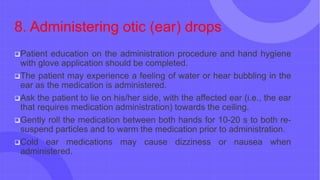
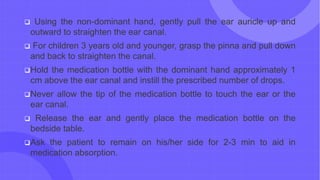
Topical drug administration involves applying medications locally to areas like the skin, eyes, ears, nose, and mucous membranes. It allows for local drug effects with fewer systemic side effects. Methods include direct application of liquids, insertions into body cavities, instillations, irrigations, and sprays. Proper topical administration requires following the rights of medication administration, preparing the application site, educating the patient, carefully applying the medication, documenting, and monitoring for side effects.