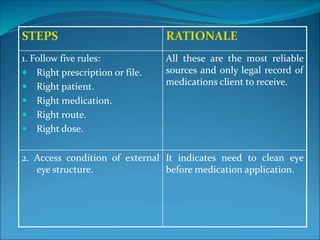
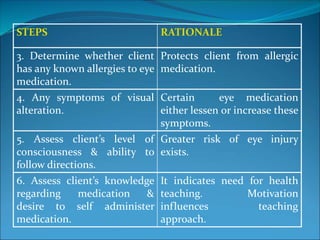
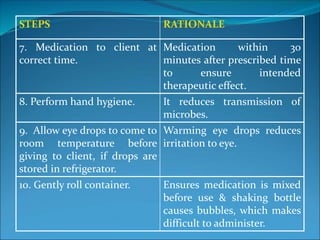
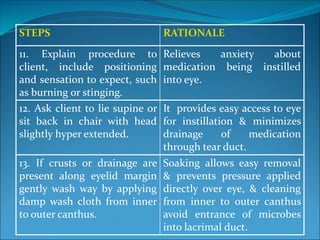
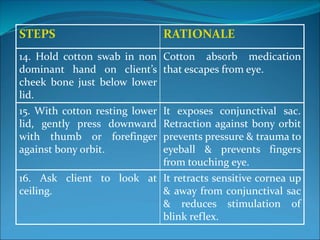
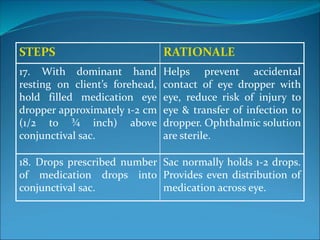
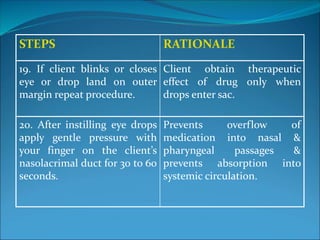
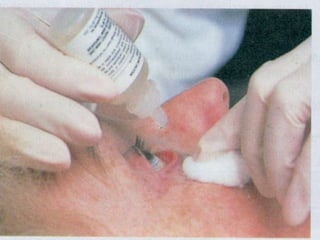
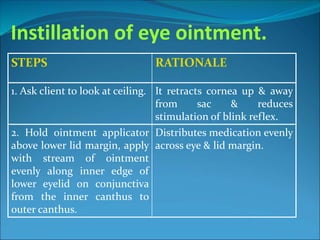
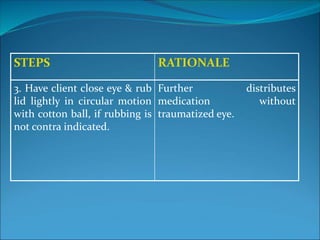
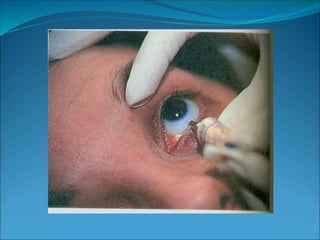
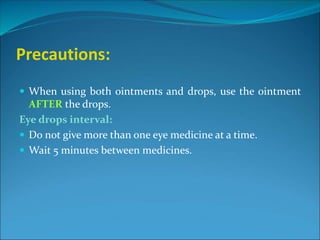
This document provides steps for properly administering ophthalmic medication. It begins by stating the importance of using the right approach and following the proper steps. It then lists 17 steps for administering eye drops, including assessing the eye, explaining the procedure to the patient, instilling the drops, and applying pressure after to prevent overflow. It also lists 3 steps for administering eye ointment and provides precautions about using ointment after drops and waiting between different eye medicines. The overall purpose is to outline the correct procedure for administering different types of eye medications to ensure maximum benefits and safety.