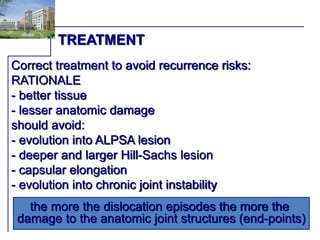
This document discusses factors related to recurrence after a first-time shoulder dislocation, including patient age and activity level, underlying pathology, and type of treatment. Younger age, overhead sports, and more severe instability patterns are associated with higher recurrence risks. Several studies found that arthroscopic stabilization surgery after a first-time dislocation significantly reduced recurrence compared to conservative treatment, especially in younger, active patients. Immediate stabilization surgery is suggested for those at high risk of recurrence.