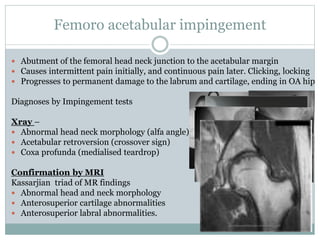
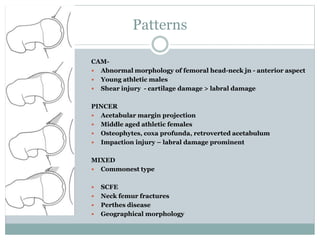
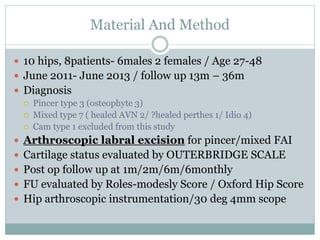
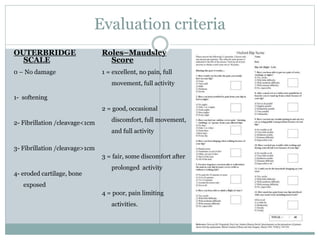
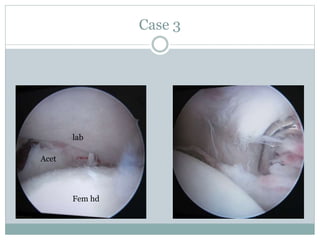
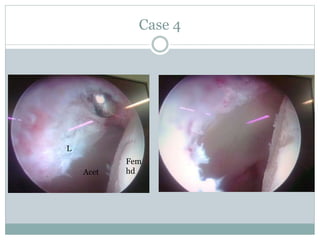
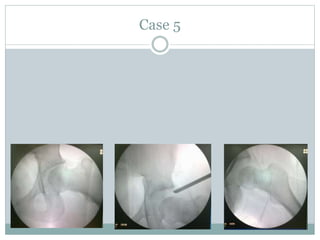
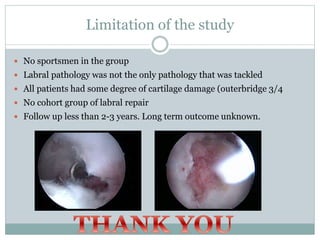
This document discusses femoro-acetabular impingement (FAI), specifically examining the role of labrectomy (labrum removal) in treatment. It presents the case that repairing a damaged labrum may not restore normal hip biomechanics, while labrectomy removes a source of pain and impingement. The author conducted a study of 10 hips that underwent arthroscopic labrectomy for pincer or mixed FAI. Post-operatively, patients showed improved clinical scores up to 2 years follow-up, indicating labrectomy provides short-term pain relief in these cases. However, the study had limitations including a lack of long-term data or comparison to labral repair techniques.