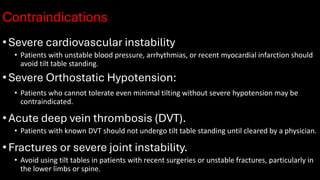
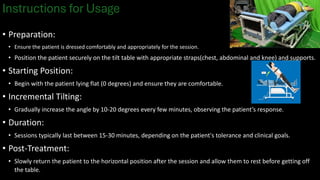
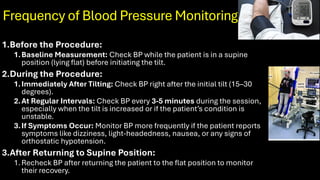
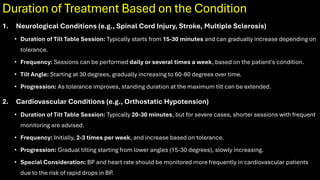
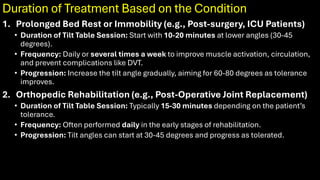
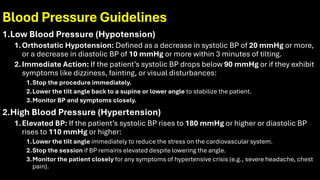
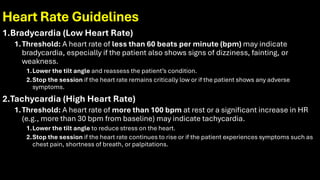
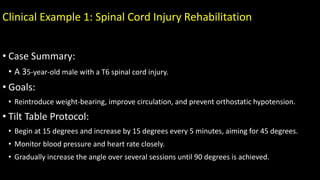
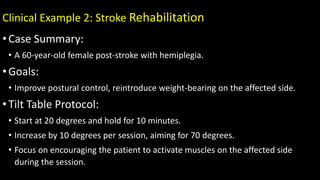
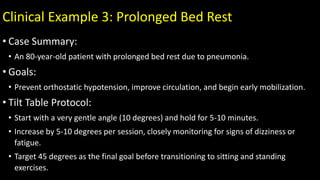
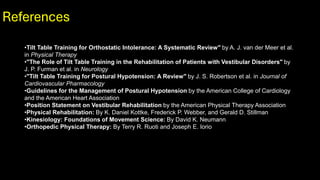
The document outlines the principles, indications, and contraindications of tilt table standing in physiotherapy, a technique used to facilitate weight-bearing and improve orthostatic tolerance in patients unable to stand independently. It emphasizes the gradual elevation of the patient, monitoring of vital signs, and specific usage instructions, including precautions based on medications and underlying health conditions. Clinical examples illustrate the application of this technique in rehabilitation for conditions such as spinal cord injuries, stroke, and prolonged bed rest.