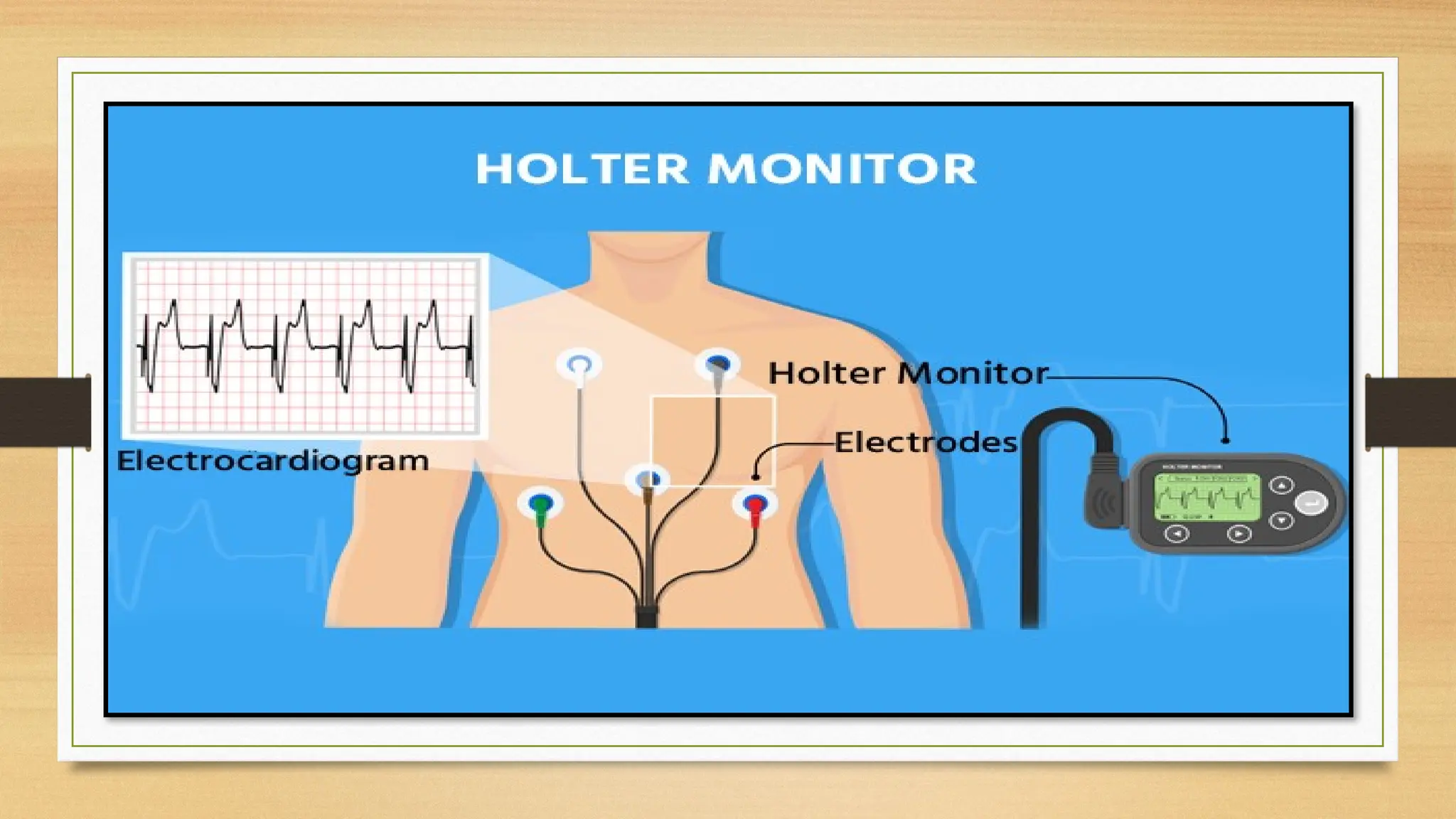
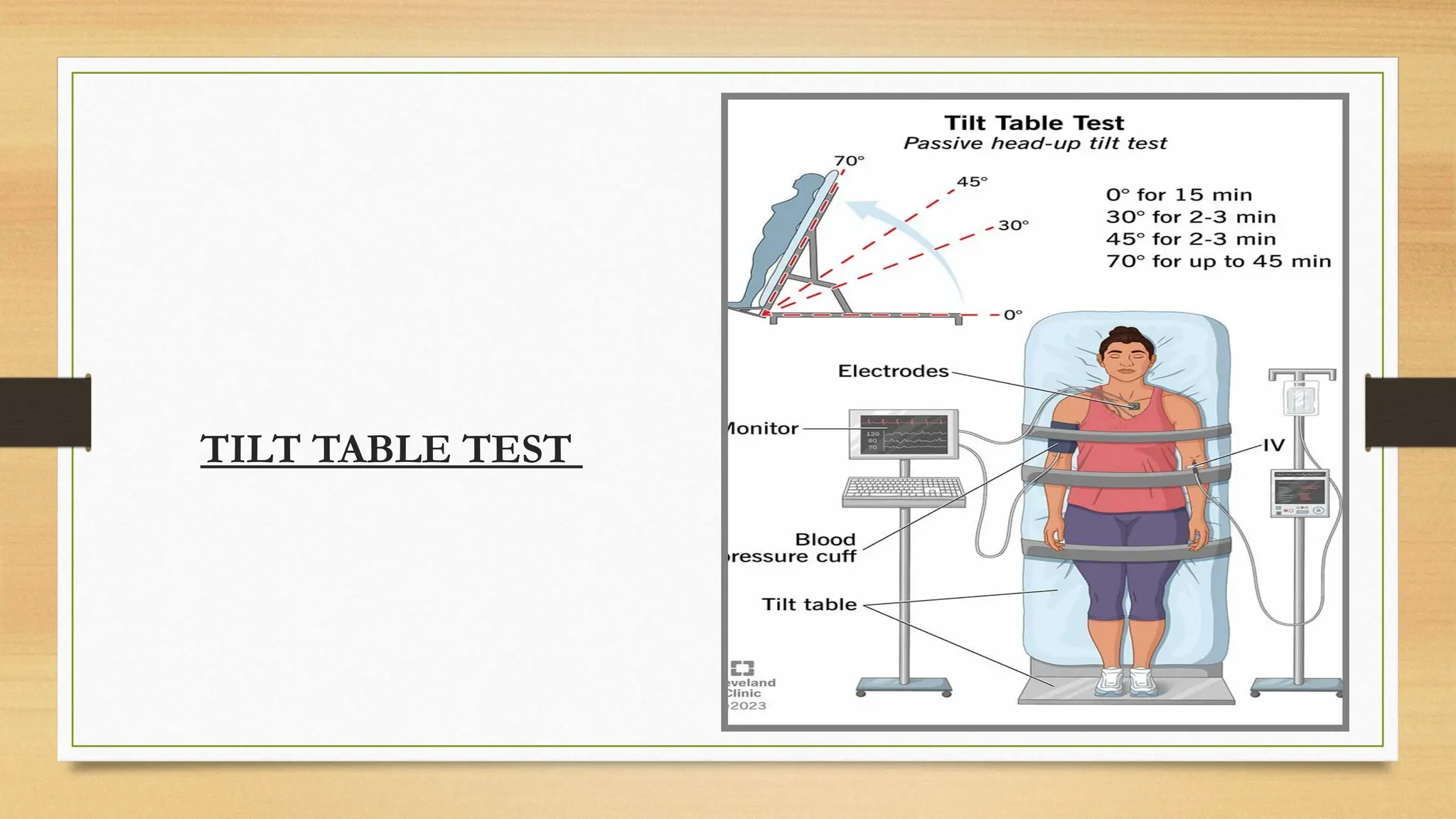
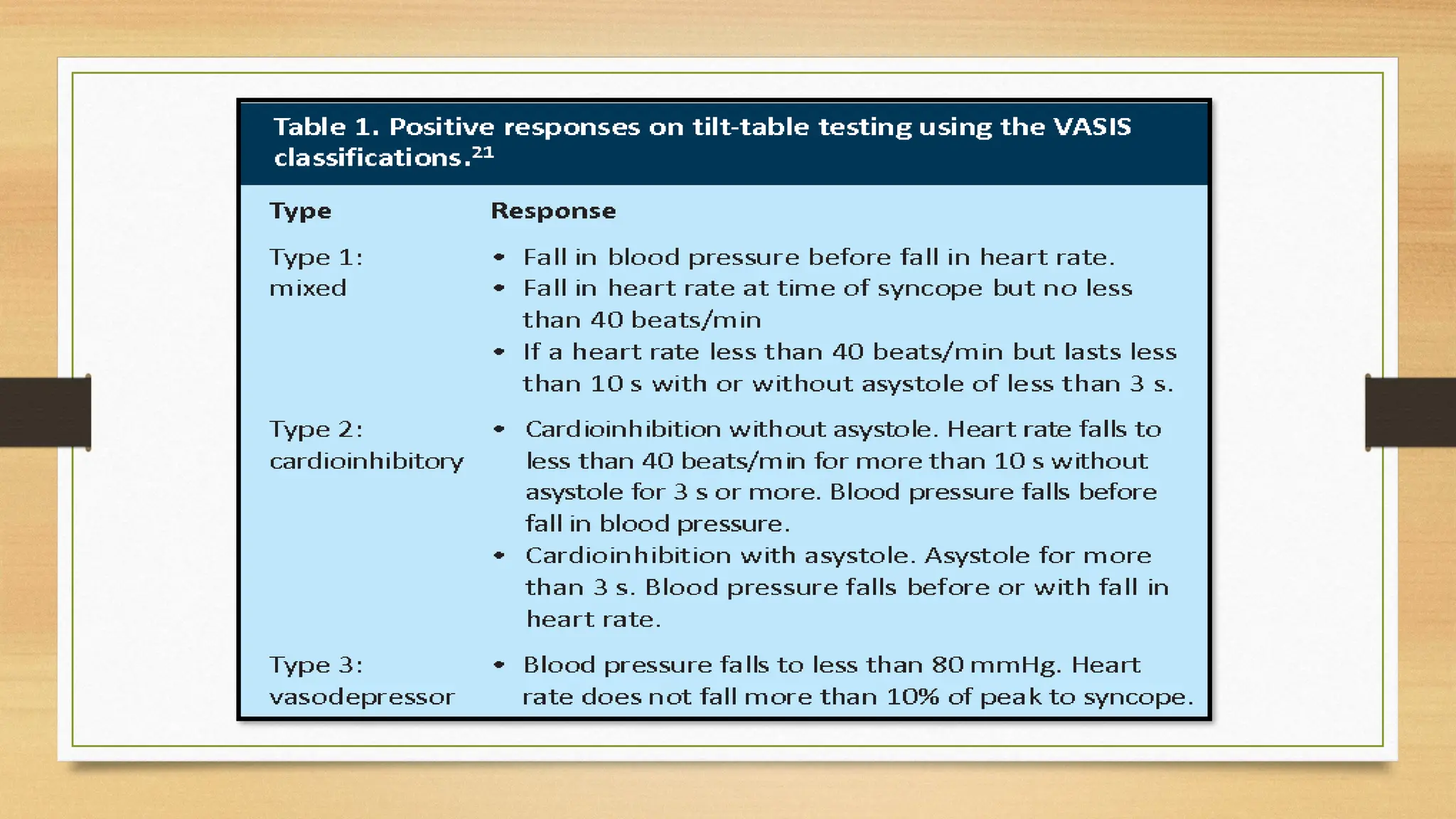
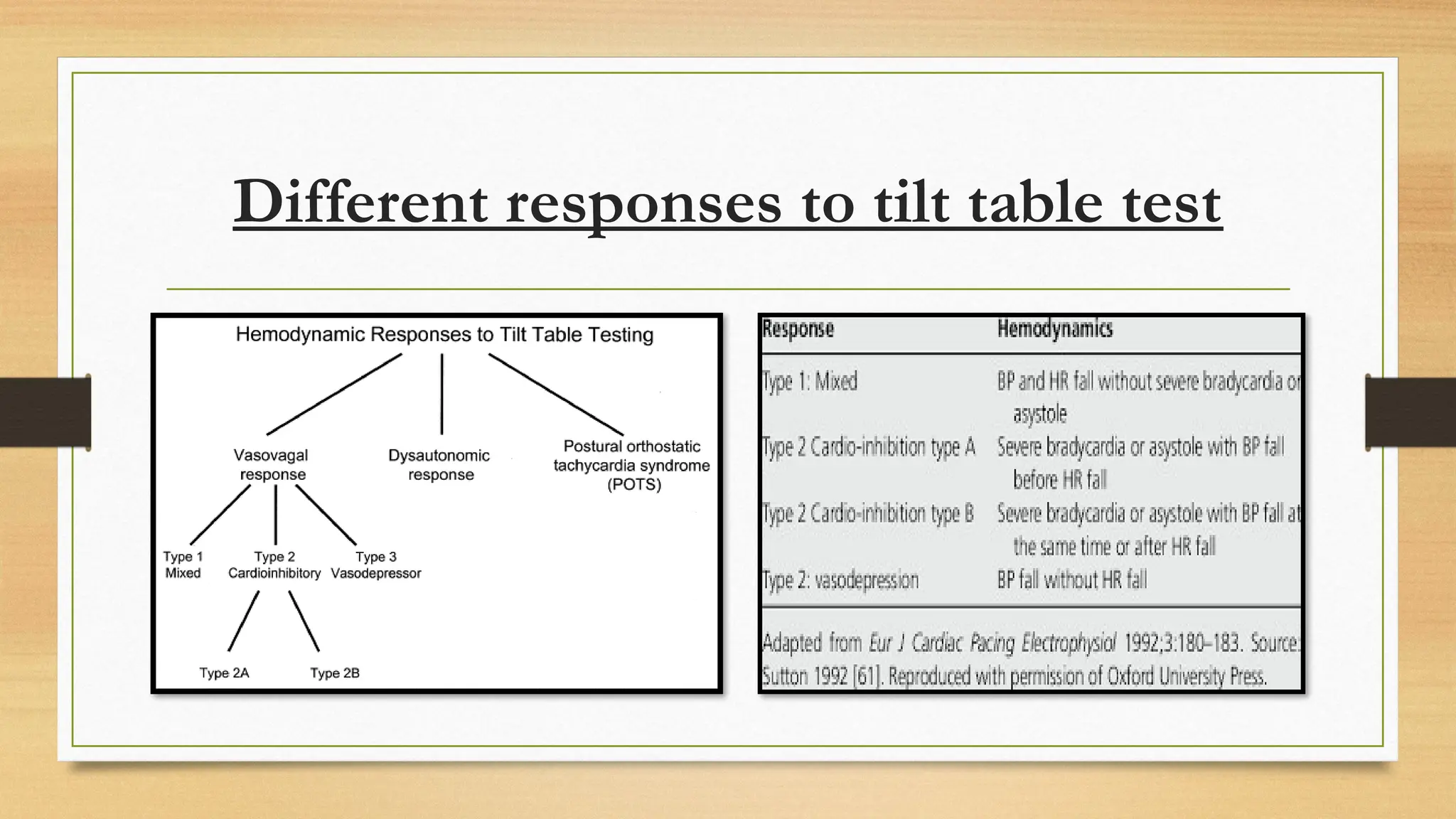
The document describes Holter monitoring, a wearable ECG device that records heart activity for 24-48 hours to identify conditions like arrhythmias and palpitations. It also explains the Tilt Table Test, which assesses blood pressure and heart rhythm responses to changes in posture, used for diagnosing syncope. Key procedures and precautions for both tests are outlined to ensure accurate results and patient safety.