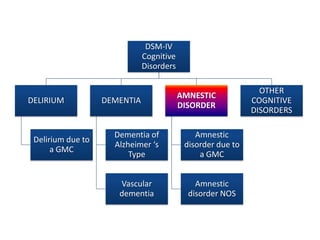
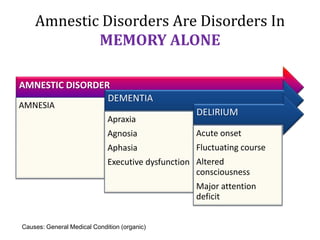
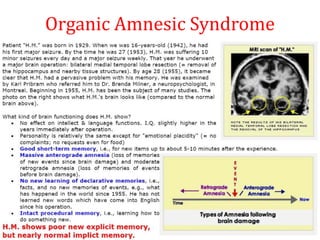
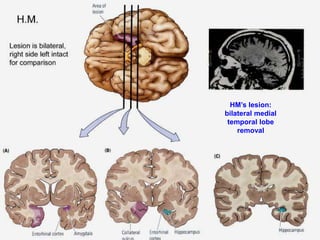
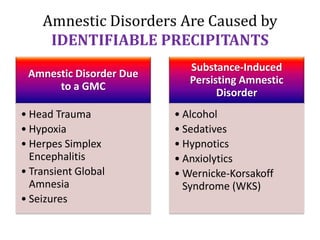
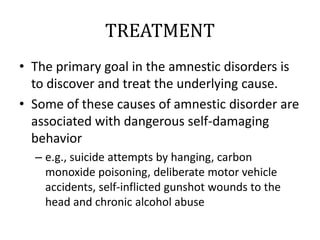
1) Amnestic disorders are characterized by memory impairment alone, most commonly caused by identifiable medical conditions that damage memory centers in the brain like the hippocampus.
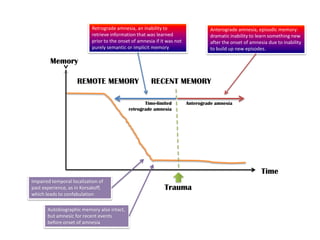
2) Organic amnesic syndrome is memory loss due to brain injury or disease, with anterograde amnesia preventing new learning and retrograde amnesia involving inability to recall events prior to the onset of amnesia.
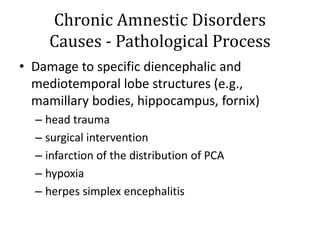
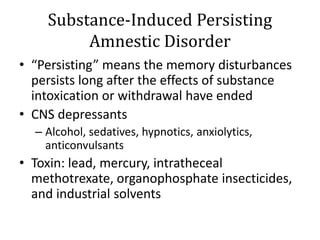
3) Common causes include alcoholism leading to Wernicke-Korsakoff syndrome, head trauma, viral infections, hypoxia, and strokes affecting memory areas like the medial temporal lobes.
![WERNICKE-KORSAKOFF SYNDROME [WKS]
CAUSES
• Alcoholism
• CO poisoning
• Encephalitis
WERNICKE
ENCEPHALOPATHY
• Delirium
• Ophtalmoplegia
• Ataxia
• Peripheral neuropathy
KORSAKOFF
SYNDROME
• Amnesia
• Confabulation](https://image.slidesharecdn.com/amnesticdisorders2013zo-170704024539/85/Amnestic-disorders-2013-16-320.jpg)
![Amnestic disorders [2013]](https://image.slidesharecdn.com/amnesticdisorders2013zo-170704024539/85/Amnestic-disorders-2013-18-320.jpg)