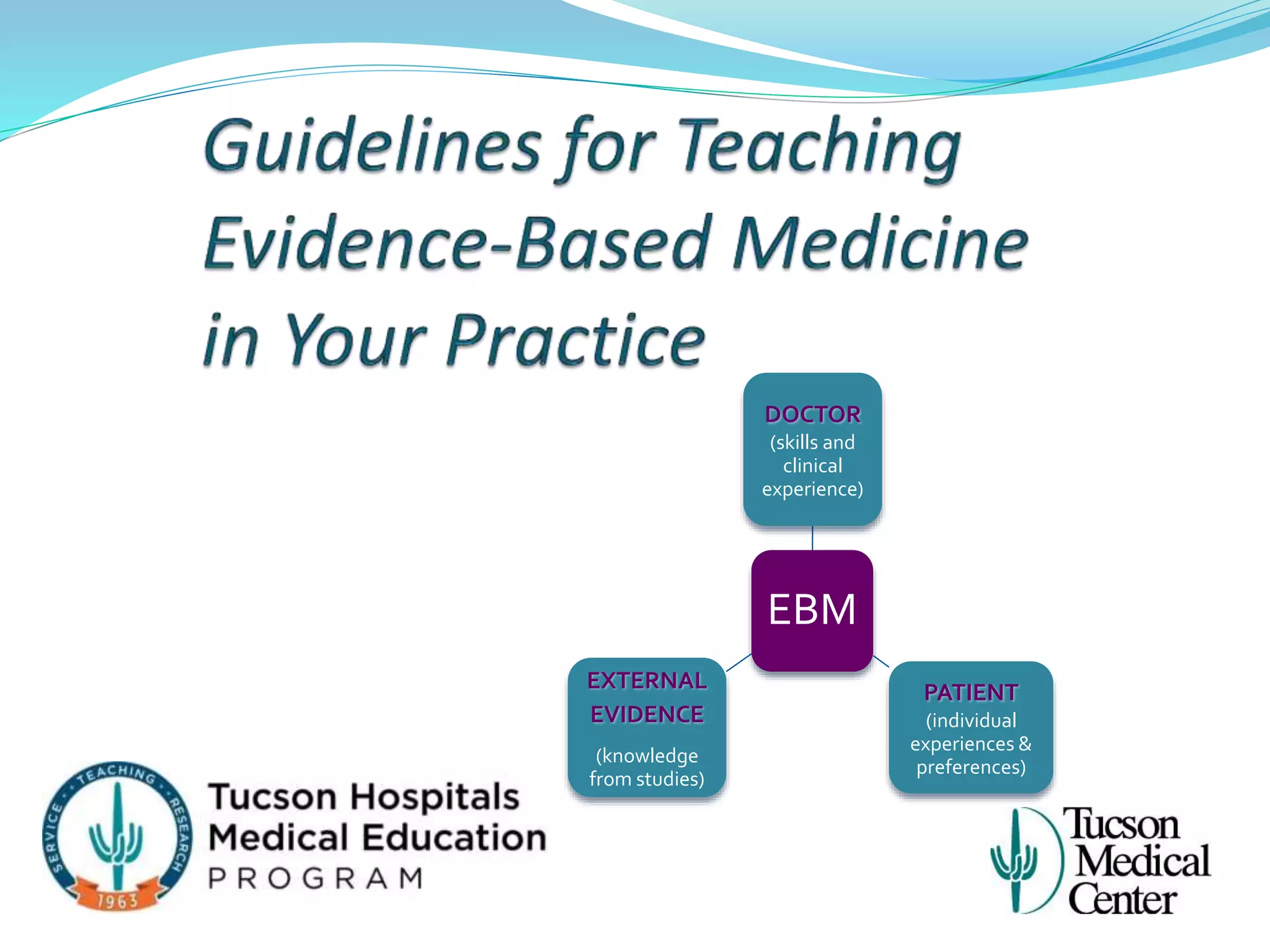
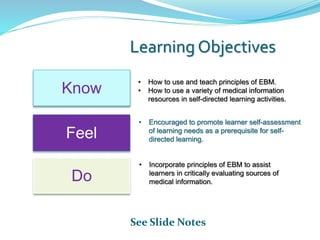
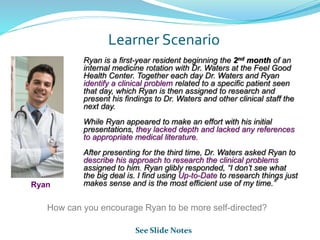
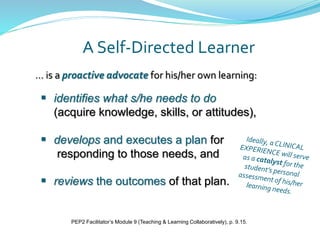
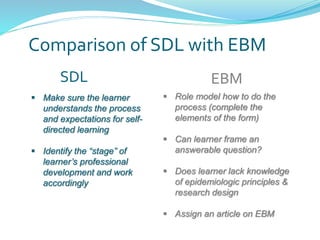
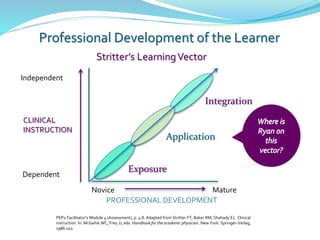
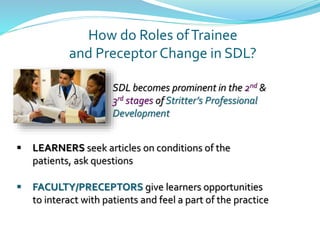
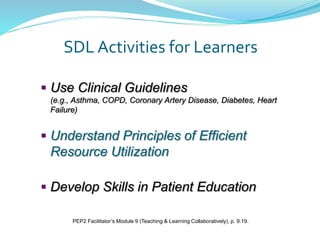
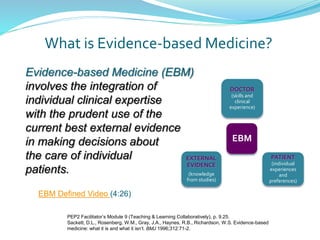
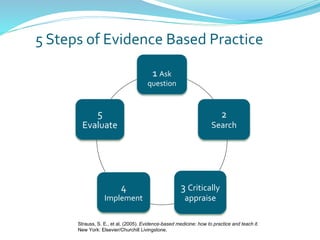
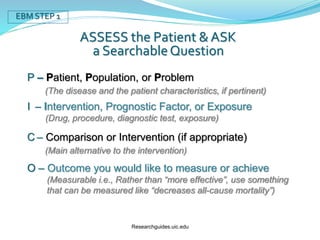
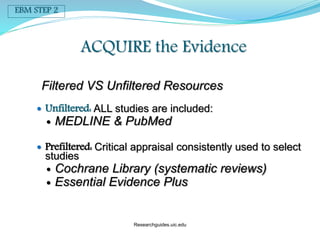
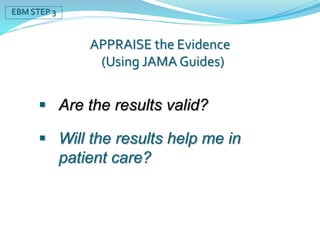
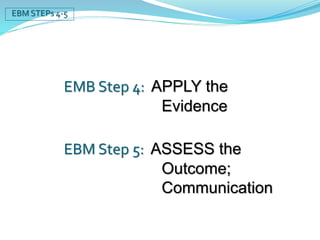
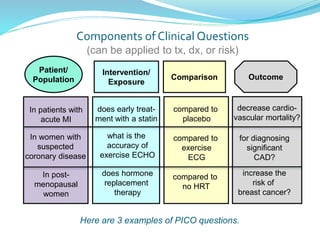
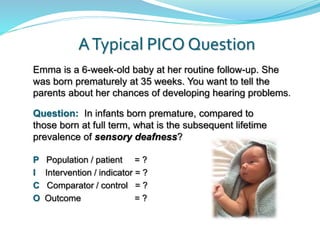
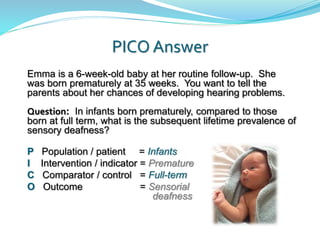
Ryan, a first-year resident, lacks depth in his clinical presentations and relies solely on UpToDate without referencing appropriate medical literature. Dr. Waters encourages Ryan to be more self-directed by following the process of evidence-based medicine (EBM). EBM involves integrating individual clinical expertise with the best external evidence from studies. Dr. Waters can role model EBM for Ryan by completing self-directed learning activities that include formulating answerable clinical questions, efficiently searching medical literature, and critically appraising evidence. Nonadherence to practice guidelines is a major barrier to successfully applying EBM.