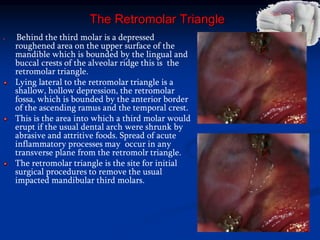
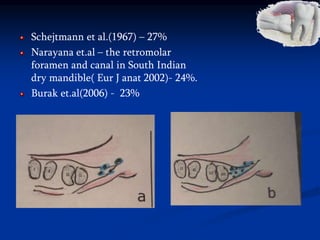
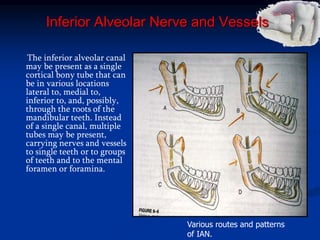
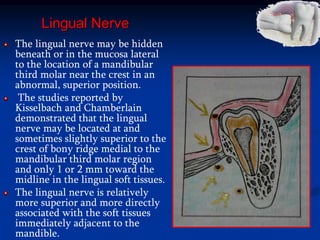
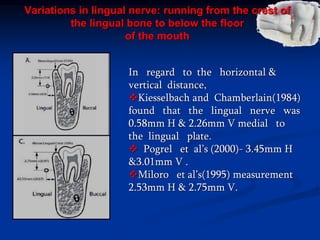
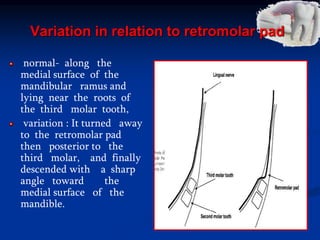
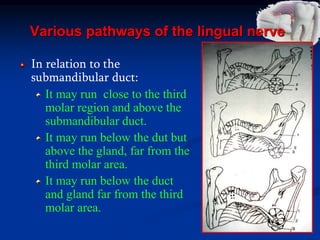
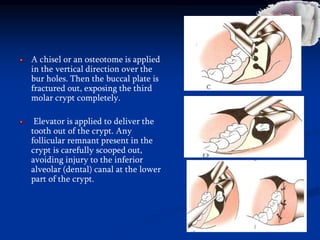
The document discusses the surgical anatomy of the mandibular third molar region. It describes the thick lateral bone and convex alveolar process medially. The mylohyoid ridge continues posteriorly towards the third molar. Behind the third molar is the retromolar triangle, bounded by lingual and buccal crests. Lateral to this is the retromolar fossa. The retromolar canal and foramen, present in around 25% of individuals, transmits neurovascular branches through this region. The inferior alveolar canal contains the inferior alveolar nerve and vessels below the third molar area.