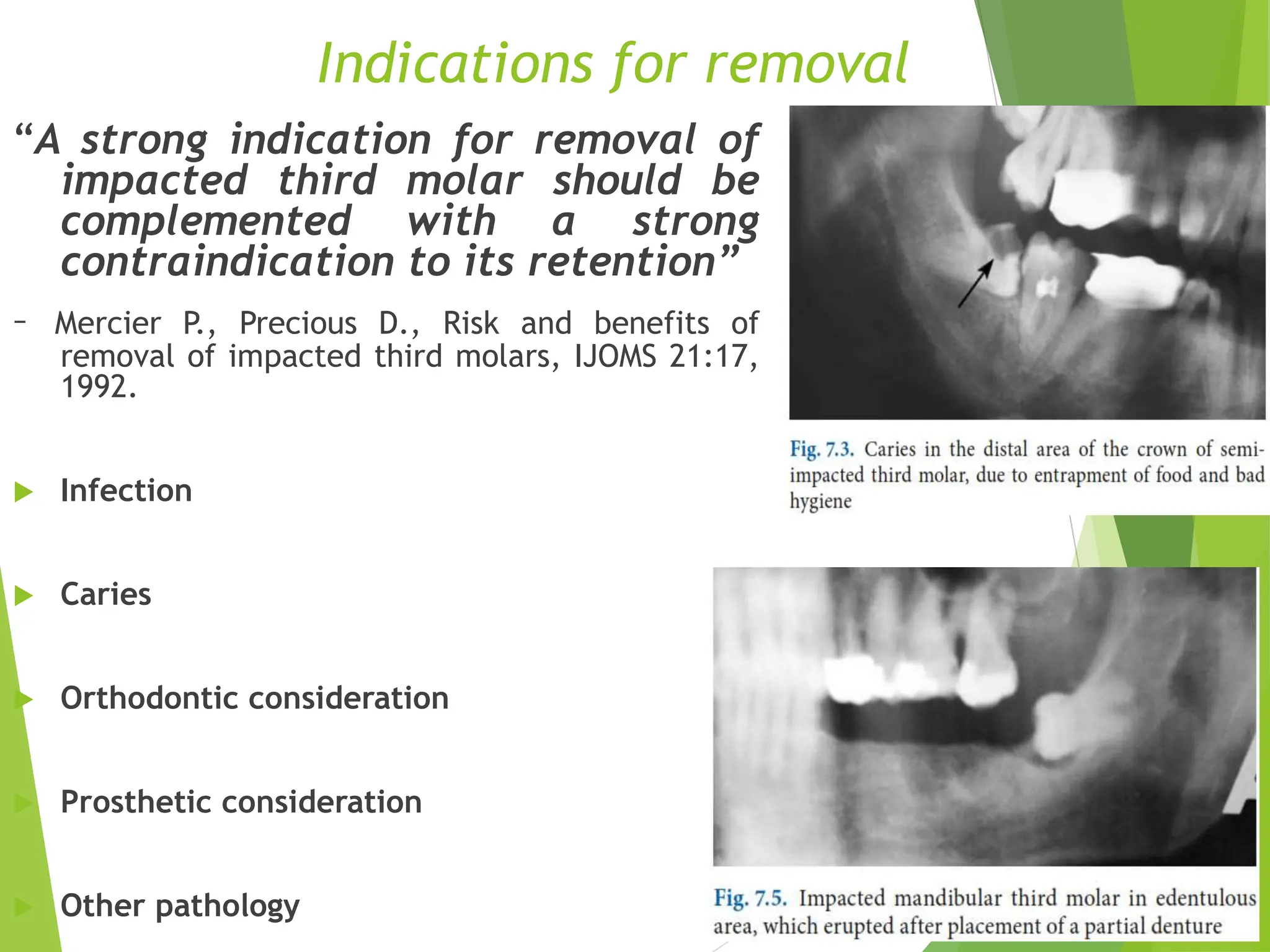
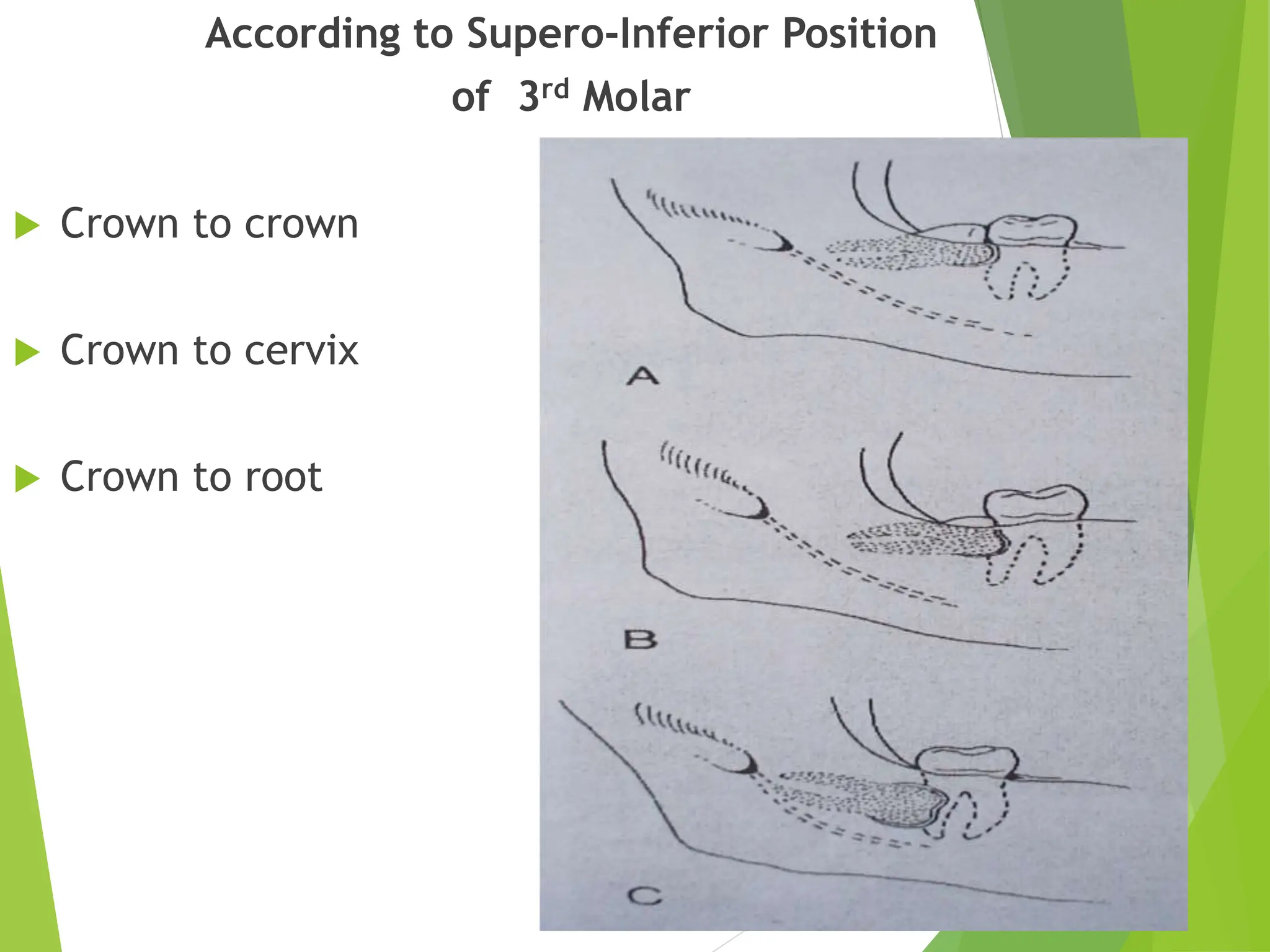
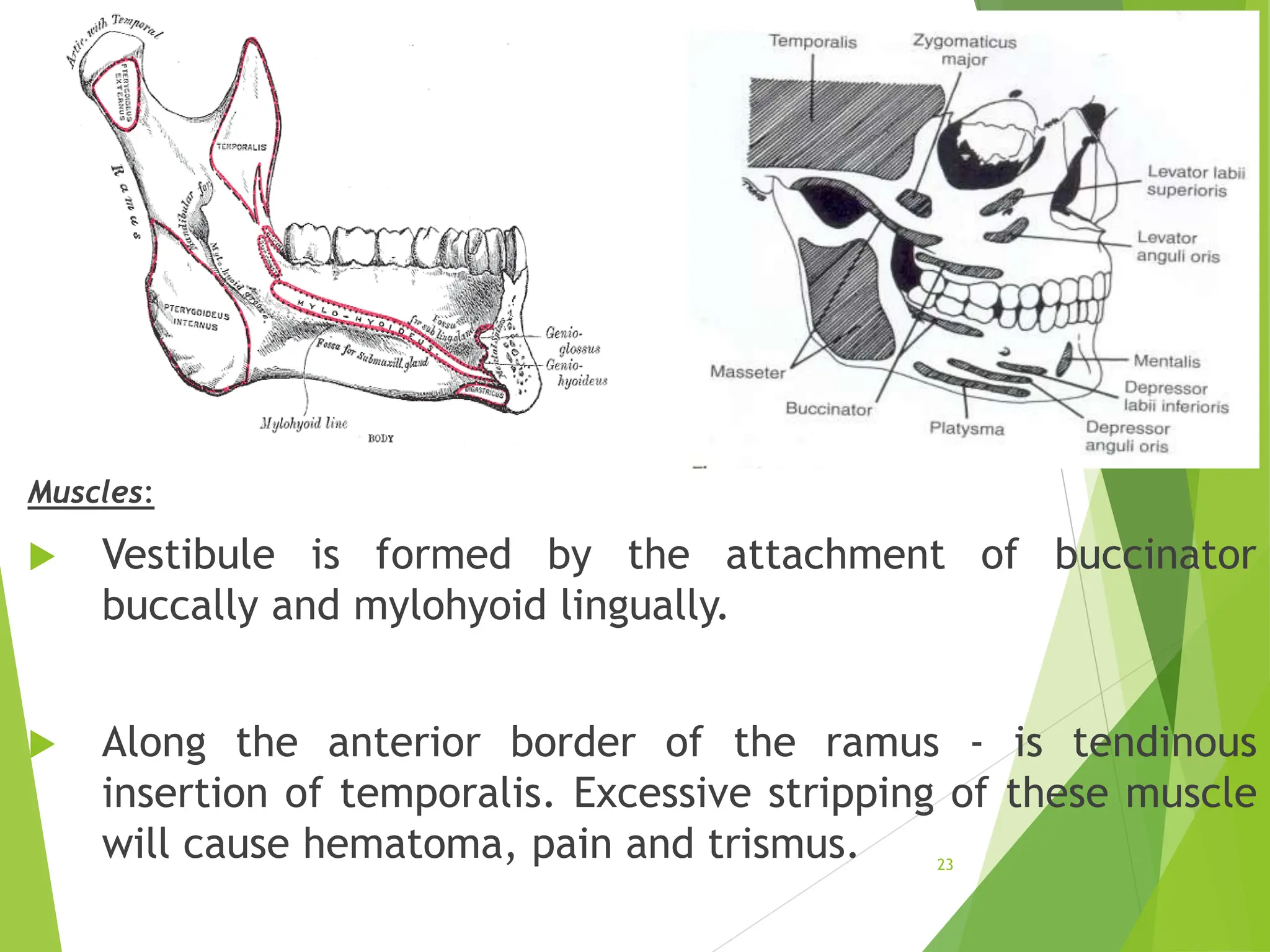
This document provides a comprehensive overview of the surgical removal of impacted third molars, addressing various topics such as definitions, theories of impaction, surgical anatomy, assessment of surgical difficulty, and potential complications. It discusses the indications and contraindications for removal, classification methods, and surgical procedures, emphasizing the importance of proper assessment and technique to minimize risks. The concluding remarks highlight the stress associated with the procedure and the need for careful consideration of each patient's unique circumstances.





![Theories of impaction
2) Phylogenic theory: Nature tries to eliminate the disused
organs i.e., use makes the organ develop better, disuse
causes slow regression of organ.
[More-functional masticatory force – better the
development of the jaw]
Due to changing nutritional habits of our civilization,
use of large powerful jaws have been practically
eliminated. Thus, over centuries the mandible and maxilla
decreased in size leaving insufficient room for third molars.
8](https://image.slidesharecdn.com/thirdmolarimpaction-240707142040-d7c205c8/75/THIRD-MOLAR-IMPACTed-tooth-development-Surgical-complications-pptx-8-2048.jpg)