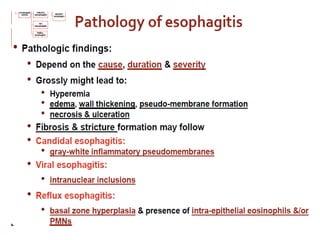
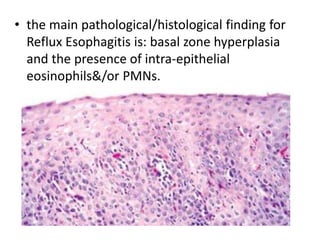
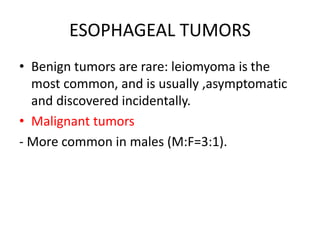
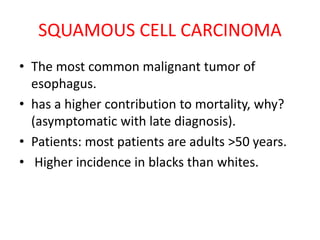
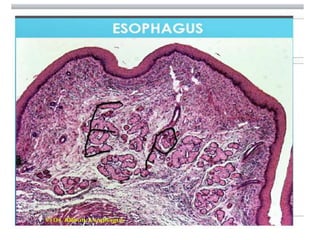
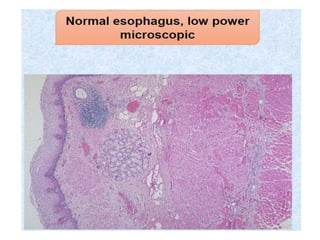
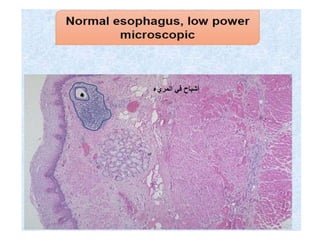
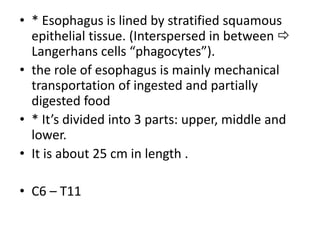
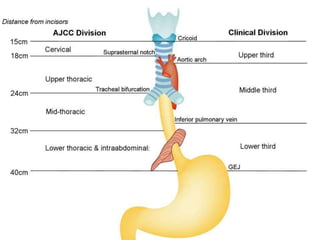
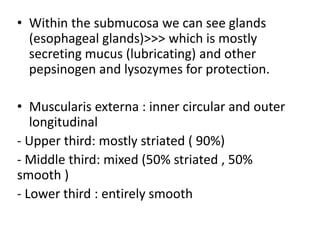
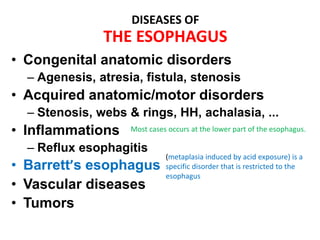
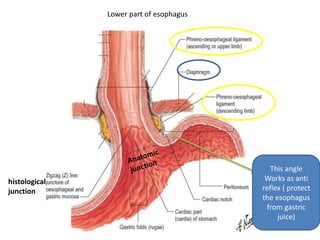
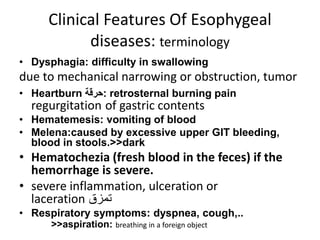
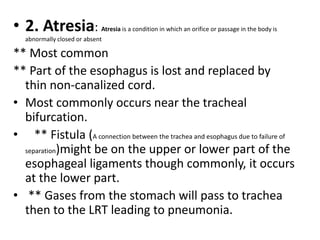
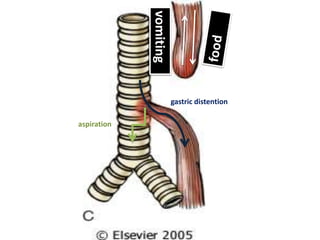
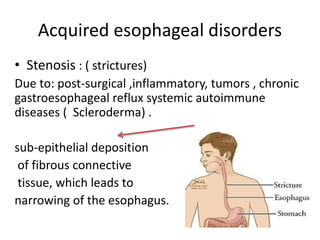
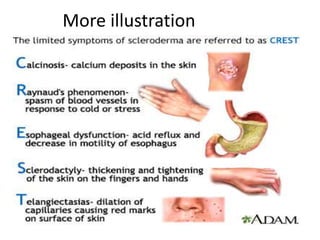
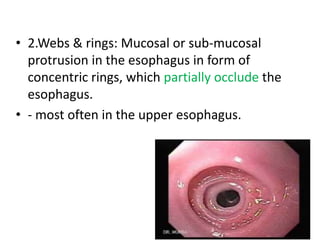
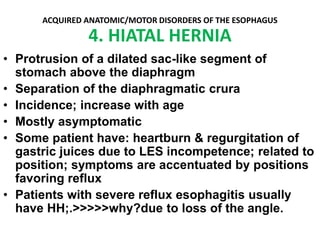
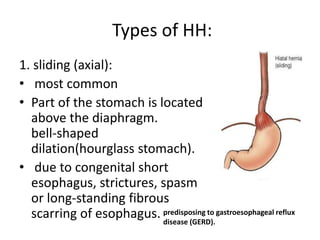
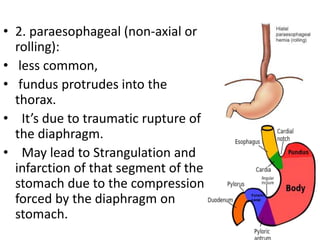
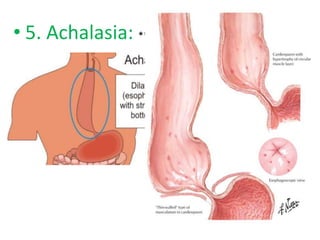
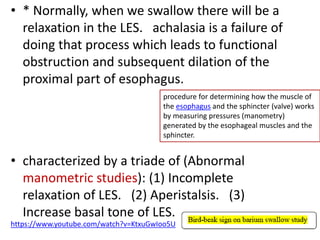
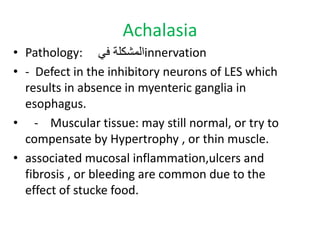
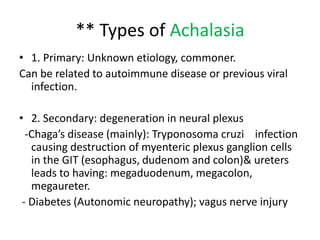
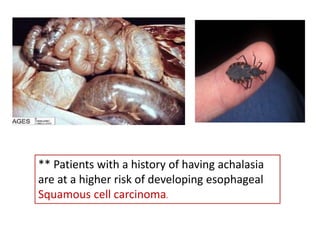
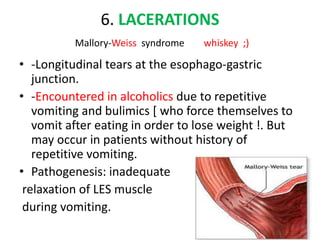
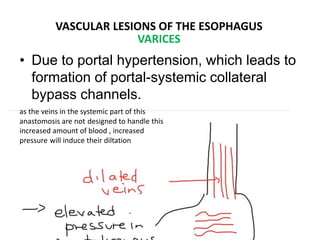
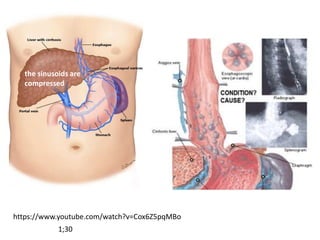
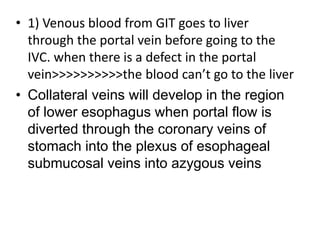
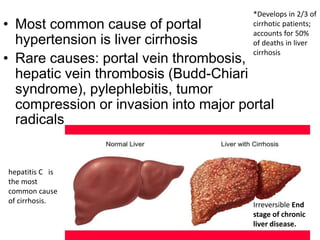
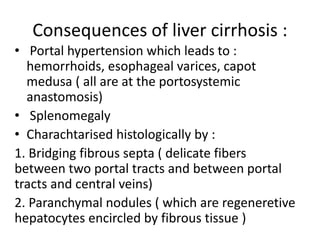
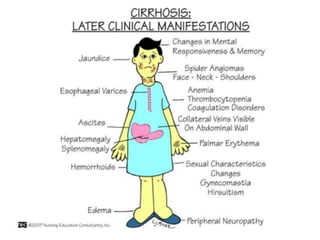
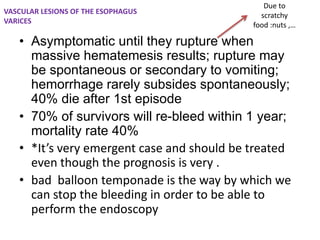
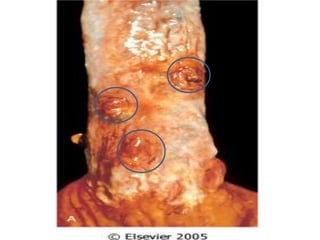
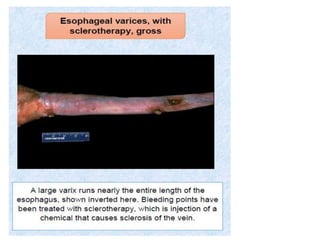
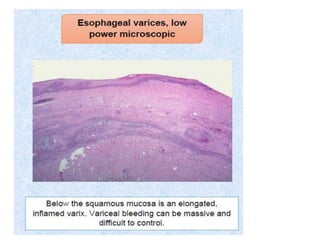
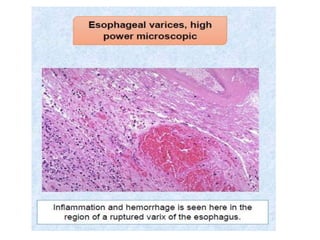
The document summarizes key aspects of the esophagus anatomy and diseases. It describes that the esophagus transports ingested food through three parts and is lined by stratified squamous epithelium. Common diseases include congenital disorders like atresia, acquired disorders like achalasia and hiatal hernia, inflammations like reflux esophagitis, and tumors. Specific conditions discussed in more detail include achalasia, where the lower esophageal sphincter fails to relax, and varices, which form due to portal hypertension in conditions like liver cirrhosis.







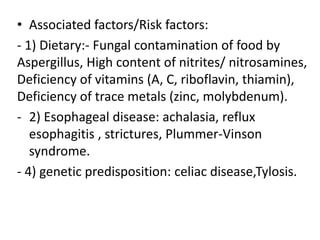
![Oesophagitis: Morson & Dawson, 5th ed, 2012
• Reflux
• Infective oesophagitis
herpes simplex
CMV
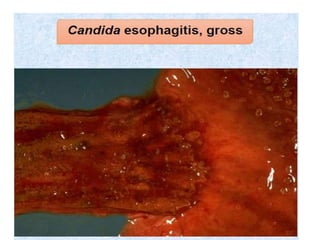
candidiasis
immunocompetent: measles, scarlet fever, diphtheria &
typhoid
immunoparetic: HIV, HZV, HPV, HHV6, varied bacteria
& fungi
• Pill oesophagitis: ferrus sulfate, (tetracyclines), NSAIDs, drugs used
for osteoporosis]
-- risk factors includes [elderly, diabetes, women (M:F = 1:2) ]
• Sloughing oesophagitis
• Eosinophilic oesophagitis
• Radiation oesophagitis
• Chagas disease](https://image.slidesharecdn.com/theesophagus-161230112404/85/The-esophagus-66-320.jpg)