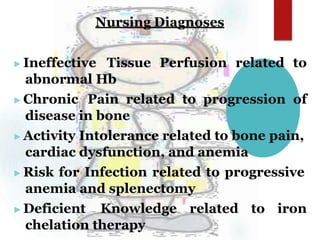
Thalassemia is a genetic blood disorder characterized by defective or reduced hemoglobin production. There are two main types: alpha thalassemia results from missing or variant genes that produce alpha globin chains, while beta thalassemia is caused by defective beta globin chain genes. Symptoms range from mild to severe anemia. Treatment depends on the severity and may include blood transfusions, iron chelation therapy, and bone marrow transplant. Prognosis is generally poor without treatment.