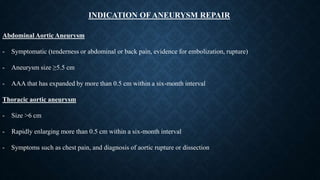
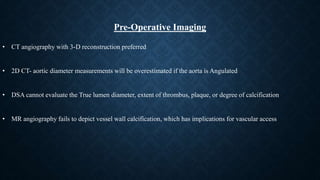
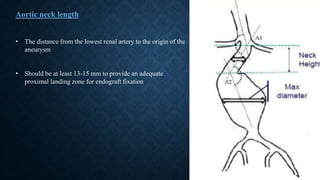
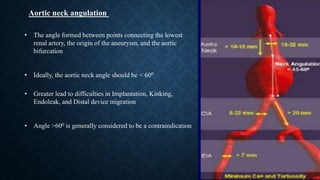
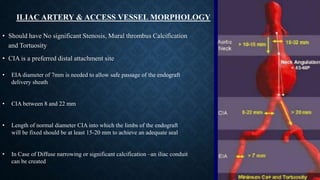
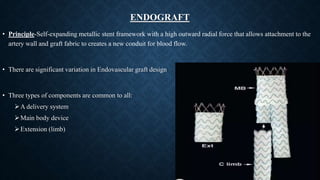
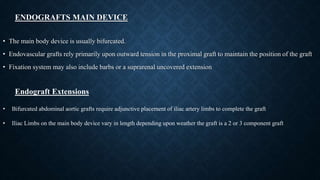
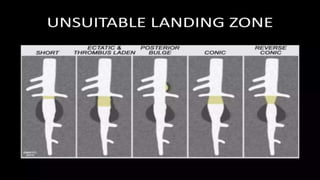
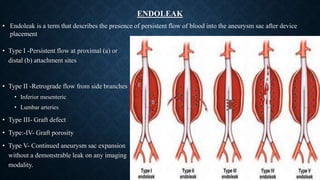
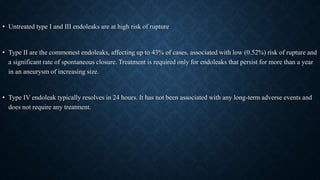
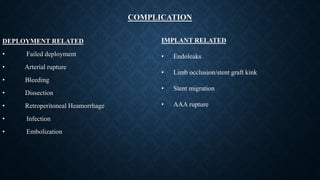
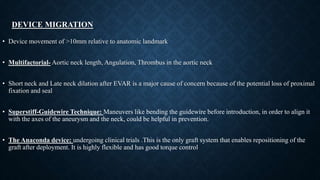
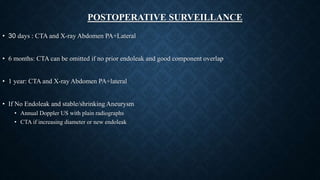
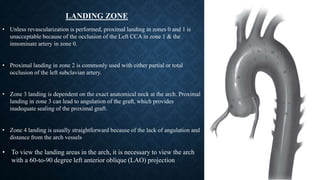
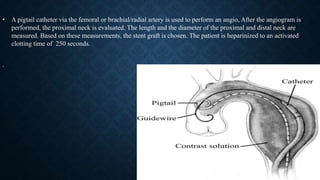
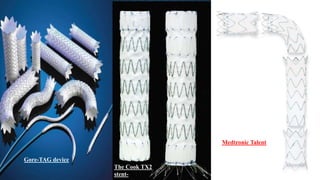
The document provides a comprehensive overview of Endovascular Aortic Repair (EVAR) and Thoracic Endovascular Aortic Repair (TEVAR), detailing their history, applications, advantages over open surgical repair, and specific indications for aneurysm repairs. It outlines pre-operative imaging techniques, the procedure steps, types of grafts used, potential complications, as well as perioperative management including patient preparation and postoperative surveillance. Key findings regarding endoleaks, device migration, and graft designs, along with guidance on imaging, access points, and procedural nuances in both EVAR and TEVAR are also discussed.