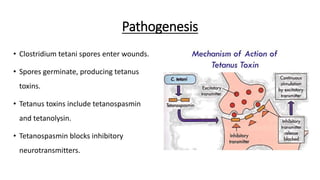
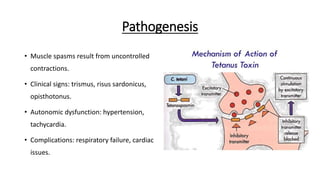
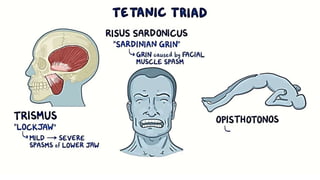
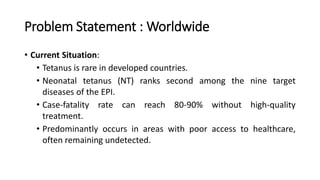
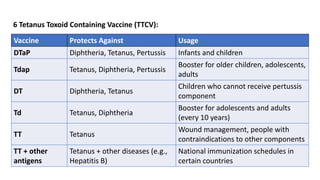
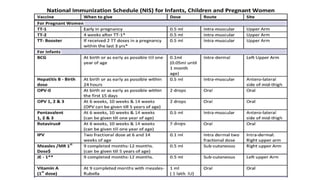
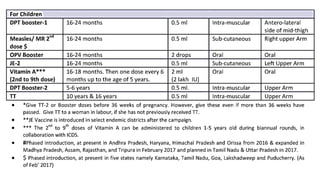
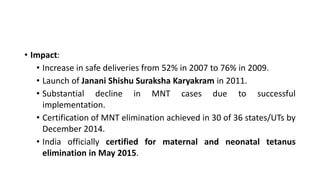
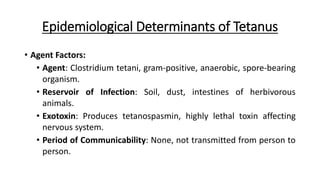
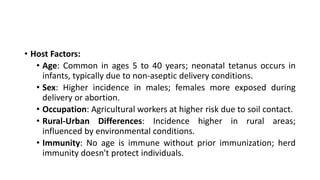
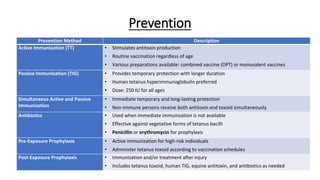
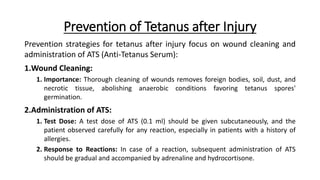
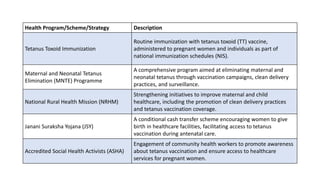
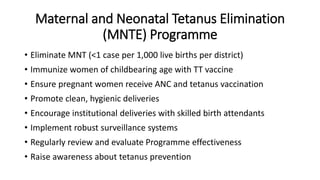
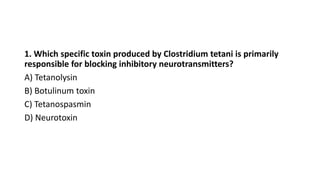
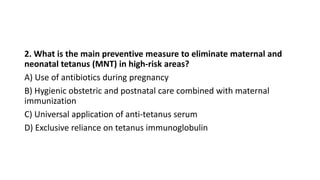
The document discusses tetanus, a severe illness caused by the Clostridium tetani bacteria, detailing its pathogenesis, worldwide challenges, and the importance of prevention through vaccination and clean practices. It highlights the success of India's maternal and neonatal tetanus elimination program, which led to a significant reduction in cases and official certification of elimination in 2015. Additionally, it outlines various health strategies and immunization schedules aimed at reducing the incidence of tetanus and ensuring maternal and neonatal health.