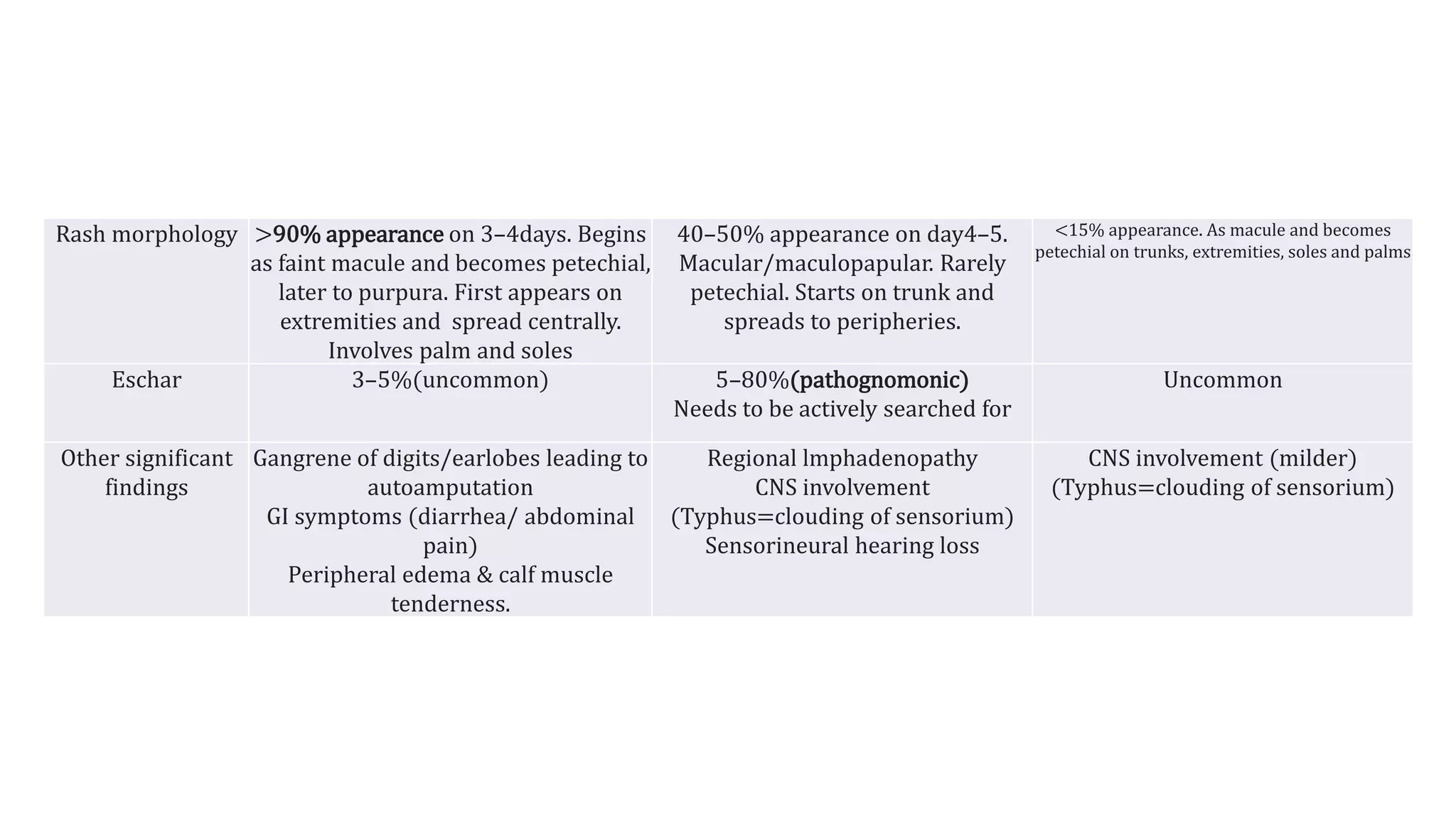
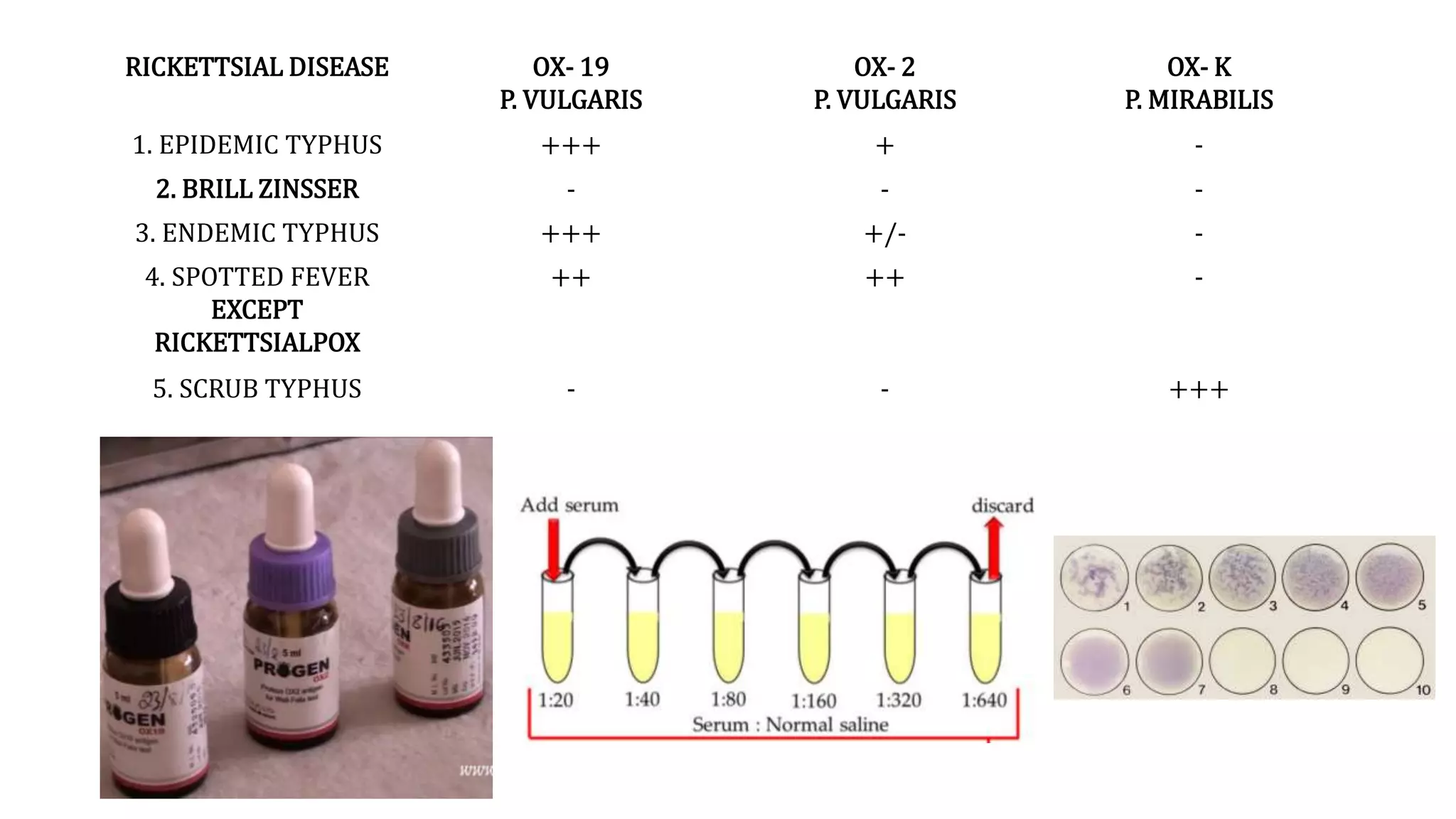
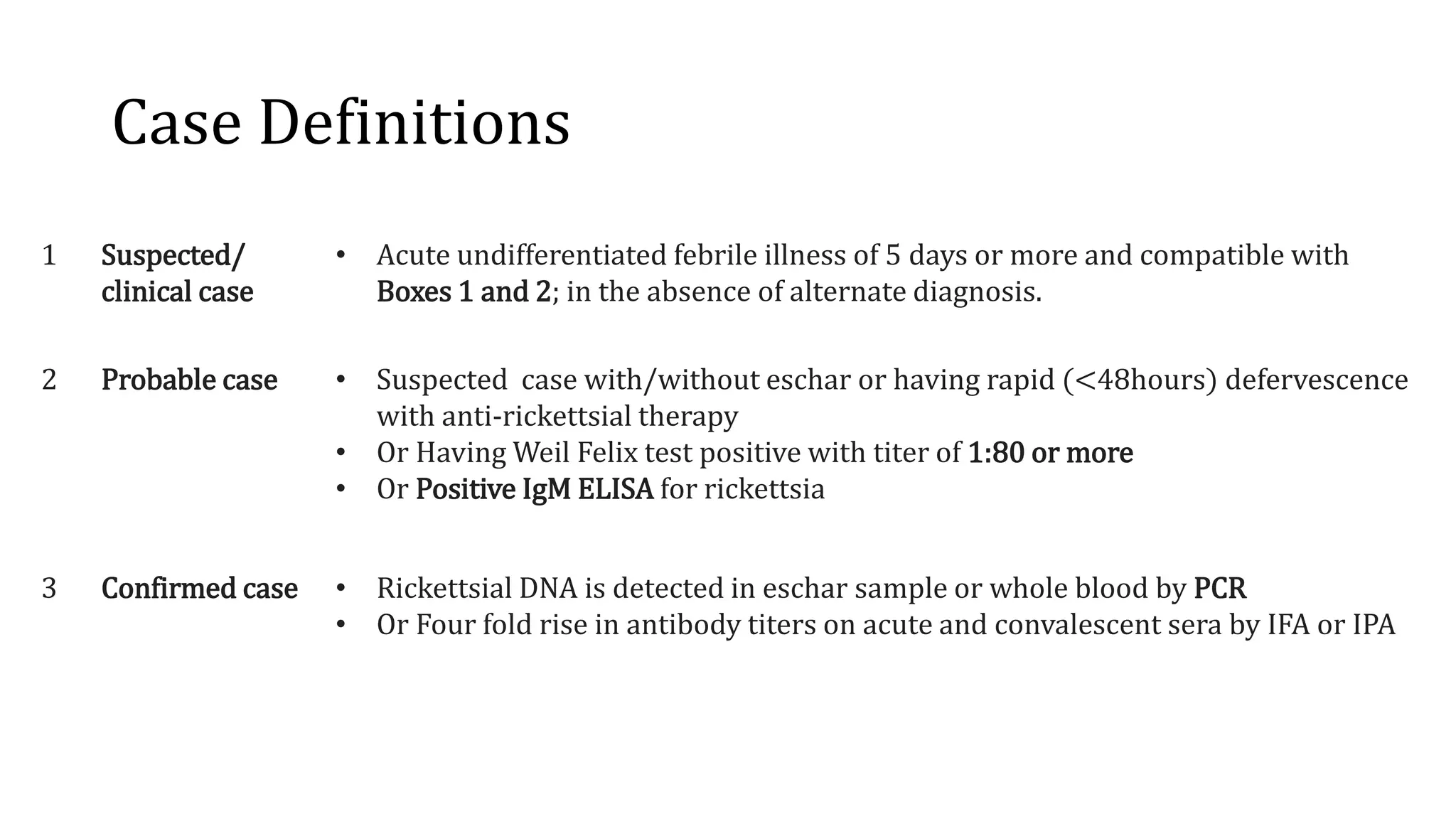
Rickettsial diseases in India are caused by gram-negative coccobacilli transmitted mainly by arthropods, with scrub typhus being the most prevalent. The clinical presentations often include fever, headache, and rashes, with varying morphological appearances, and can lead to severe complications if untreated. Diagnosis relies on clinical suspicion supported by epidemiological data and laboratory tests, while immediate empiric treatment with doxycycline is recommended upon suspicion of infection.