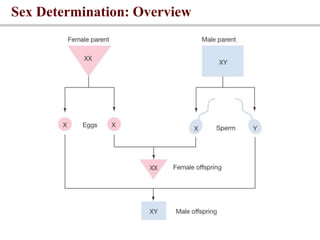
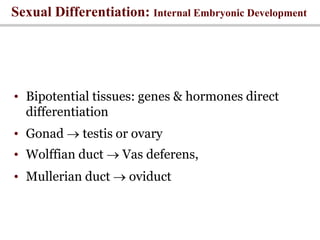
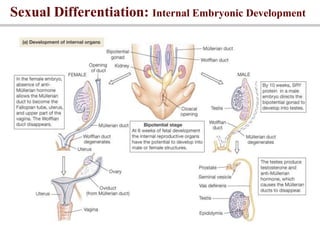
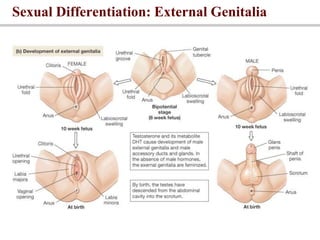
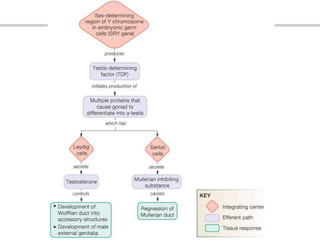
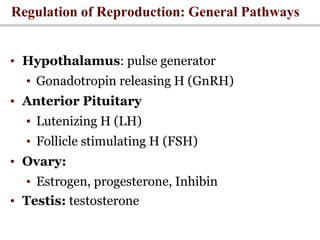
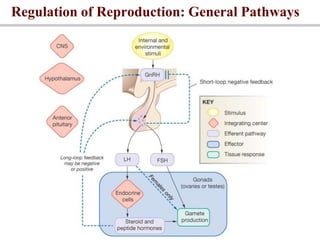
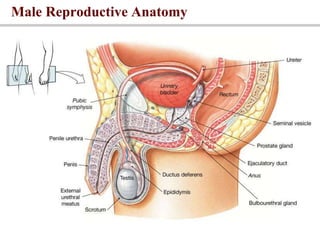
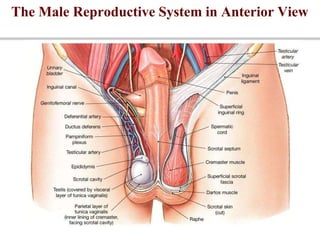
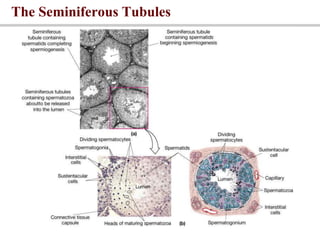
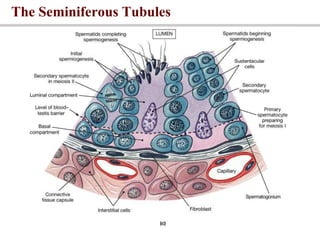
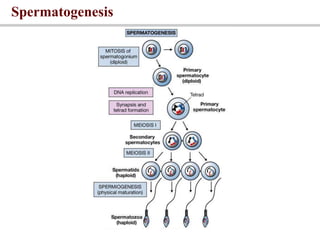
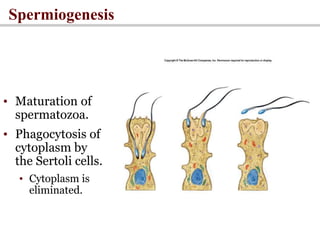
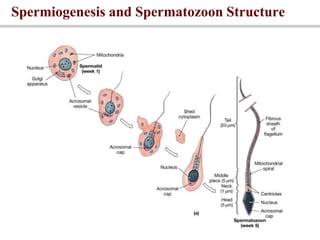
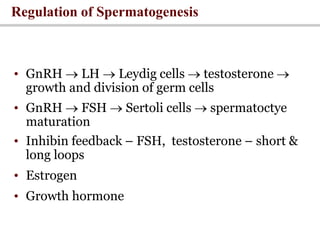
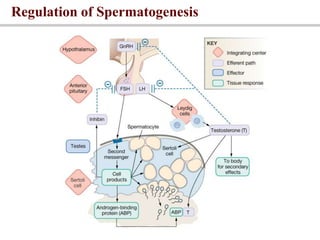
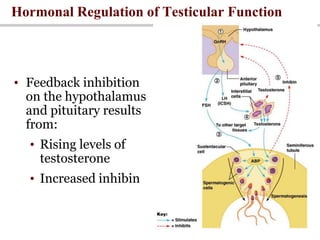
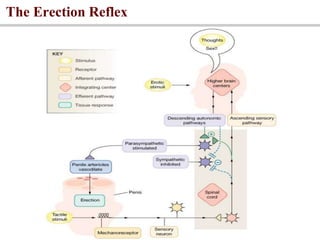
The document discusses the male reproductive system. It covers sex determination in embryos, development of internal and external genitalia, and the anatomy and physiology of the male reproductive tract. This includes the testes, epididymis, vas deference, seminal vesicles, prostate, and penis. It also summarizes the hormonal regulation of reproduction by the hypothalamus, pituitary, and gonads. Key points are the roles of FSH, LH, testosterone, and other hormones in spermatogenesis and sexual function in males.