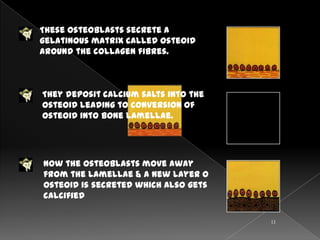
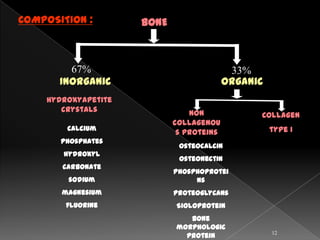
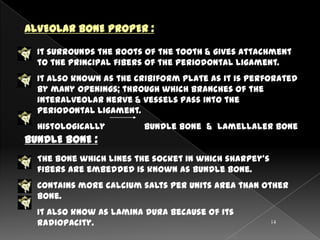
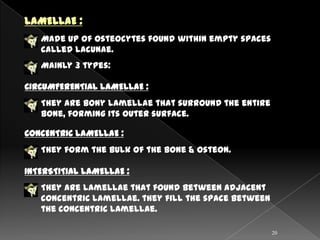
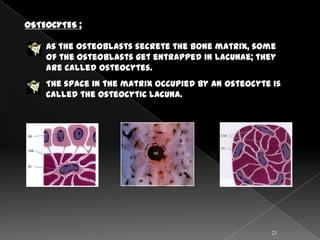
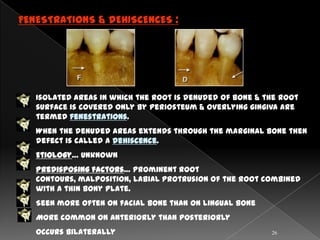
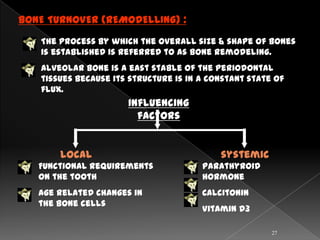
The document discusses the alveolar bone, including its definition, composition, structure, cells, blood supply, and changes associated with orthodontic forces. It notes that alveolar bone surrounds and supports the teeth sockets. It is composed primarily of inorganic minerals and collagen. Microscopically, it contains osteons arranged in concentric lamellae around Haversian canals. Osteoblasts build bone while osteoclasts resorb it, maintaining a constant state of remodeling. The alveolar bone has a rich blood supply from the superior and inferior alveolar arteries and drains via lymph vessels. Orthodontic forces induce changes in the bone's morphology and turnover.