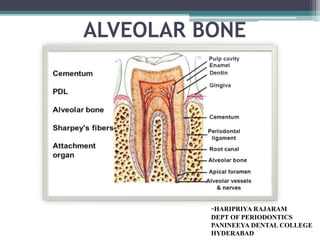
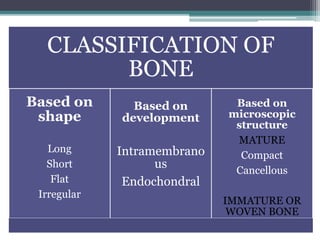
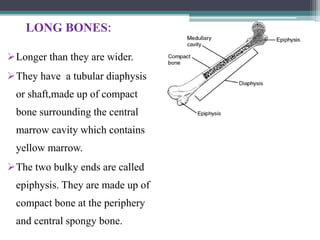
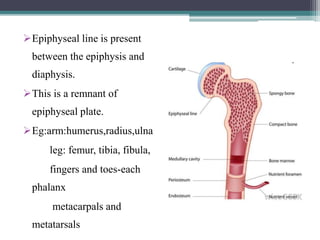
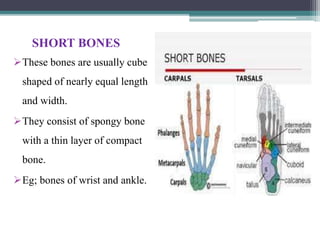
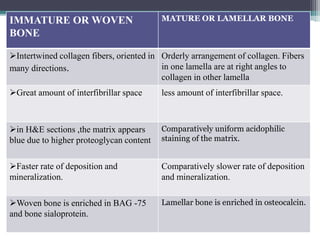
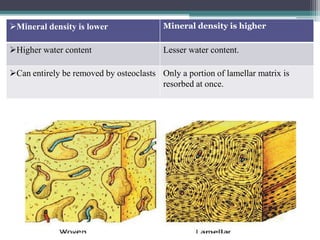
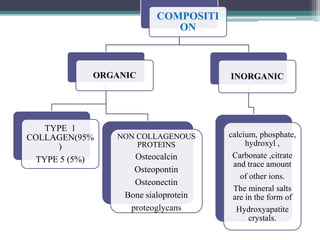
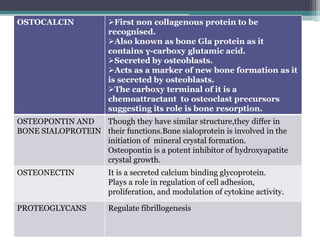
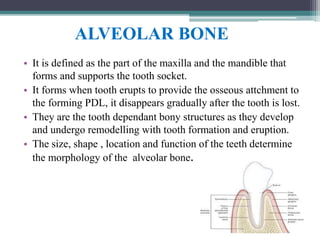
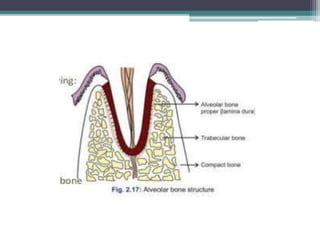
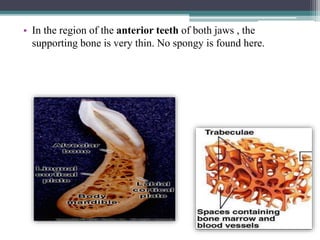
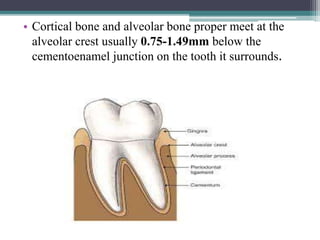
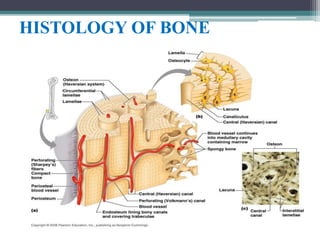
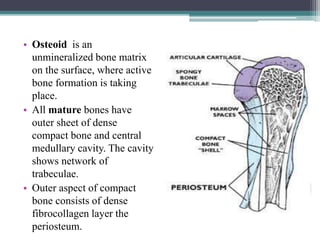
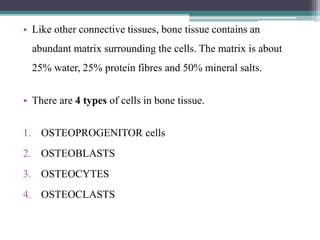
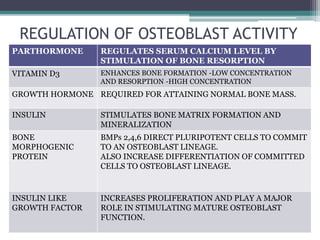
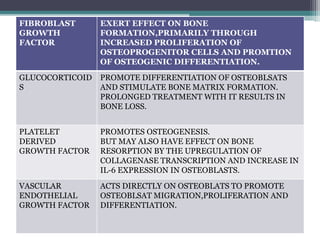
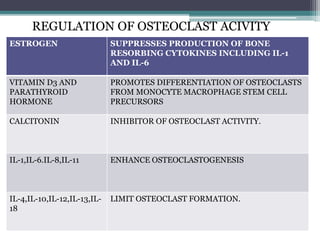
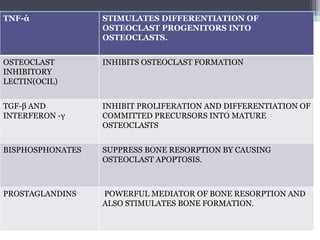
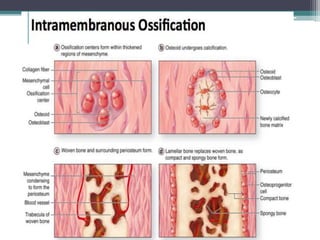
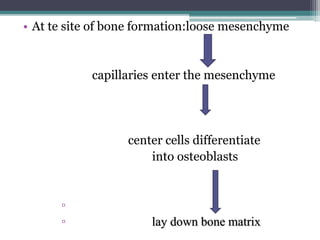
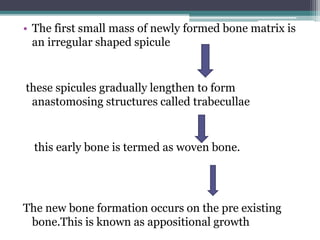
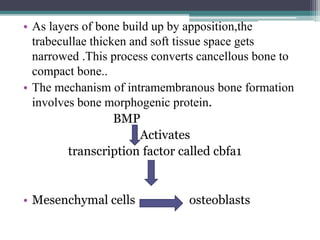
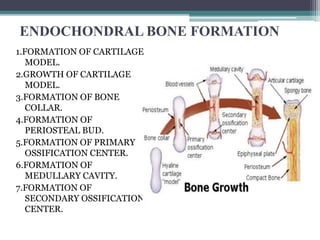
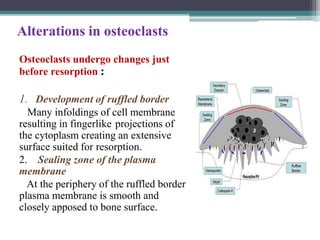
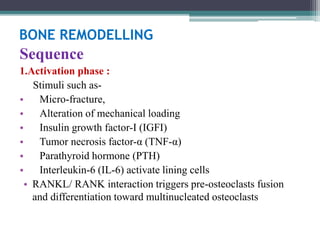
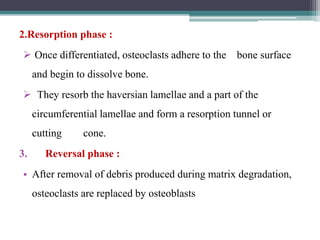
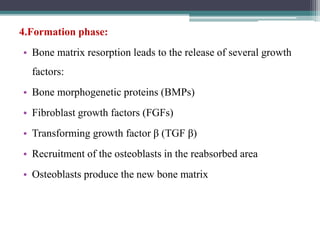
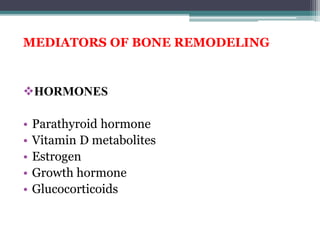
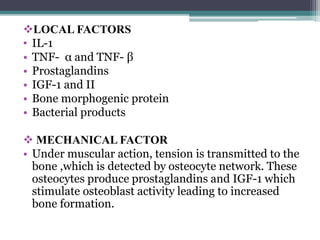
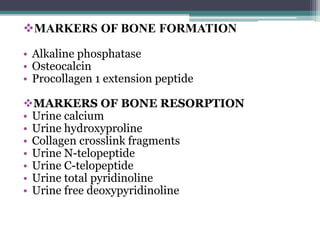
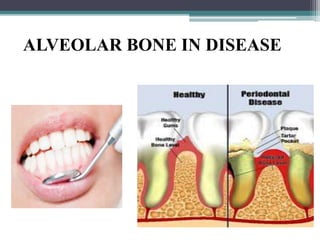
This document provides a comprehensive overview of alveolar bone, including its anatomy, classification, composition, histology, and functions. It details bone formation processes, types of bone, the role of different cells involved in bone metabolism, and the clinical implications of alveolar bone health. The document highlights the importance of alveolar bone in supporting teeth and its dynamic nature in response to dental and physiological changes.