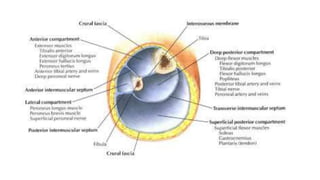
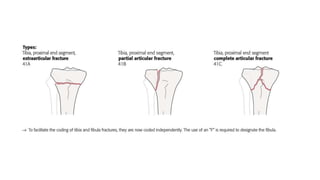
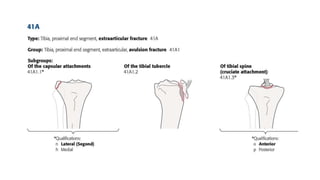
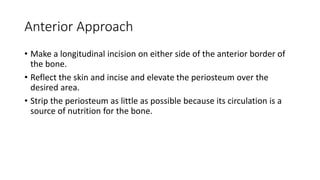
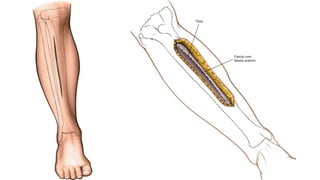
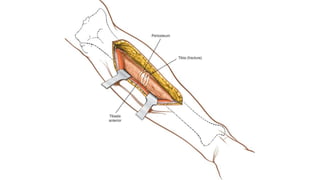
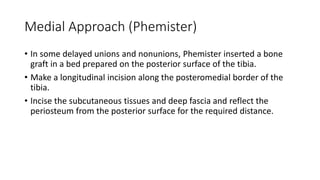
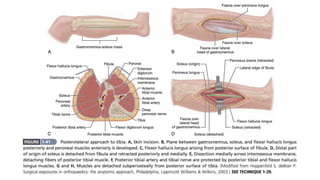
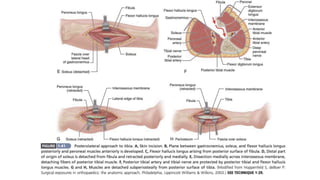
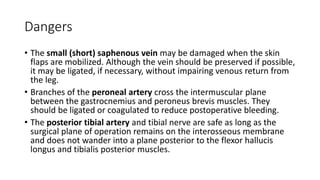
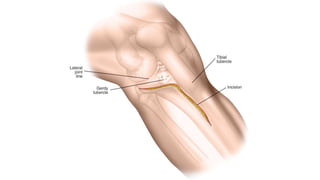
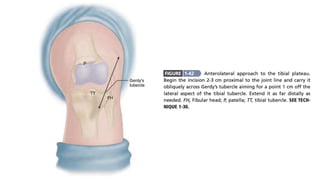
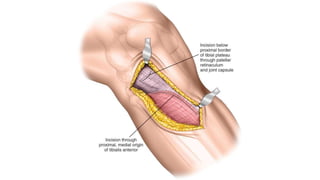
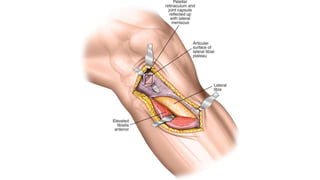
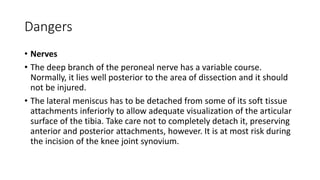
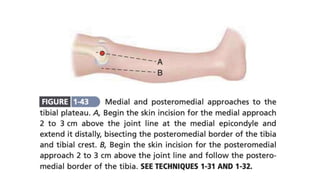
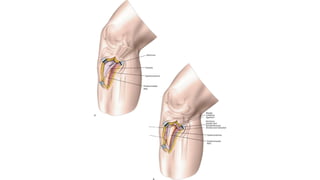
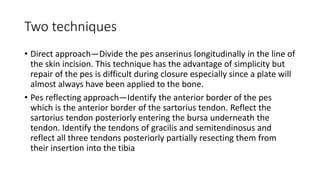
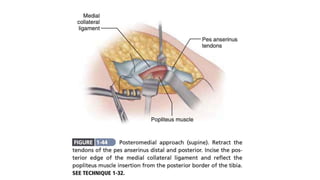
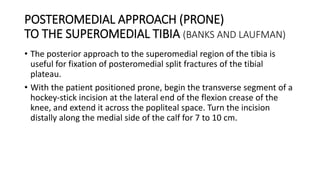
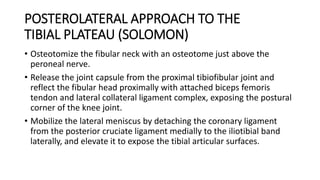
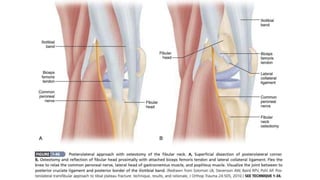
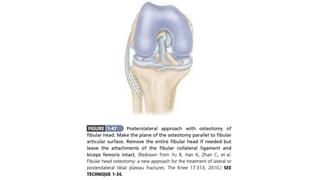
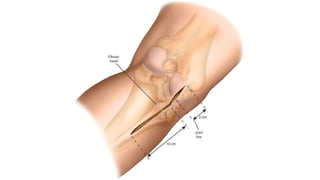
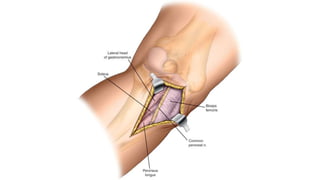
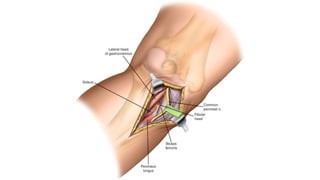
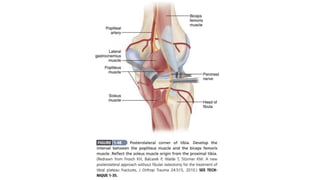
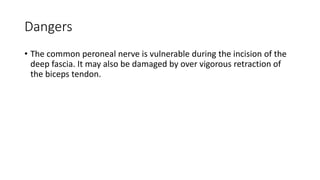
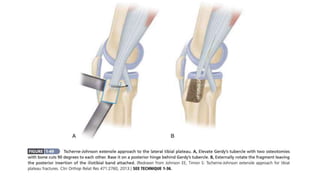
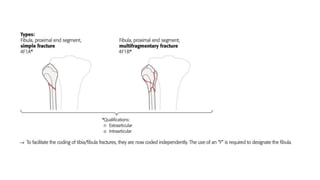
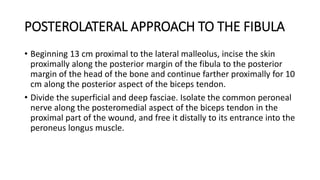
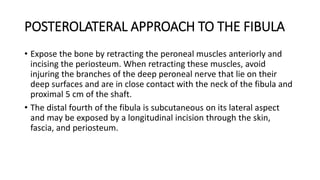
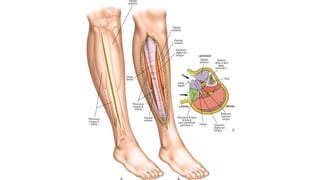
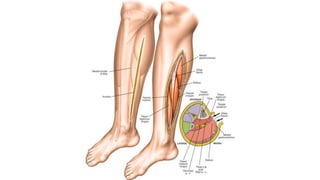
This document describes several surgical approaches for the tibia and fibula. It discusses anterior, medial, posterolateral, and posteromedial approaches for the tibia. It also covers anterolateral, medial, posteromedial, posterolateral, and Tschern-Johnson extensile approaches for the tibial plateau. Each approach is described in detail, including incision location, tissue dissection steps, indications, and potential dangers.