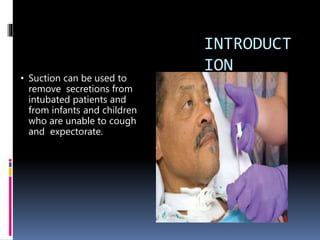
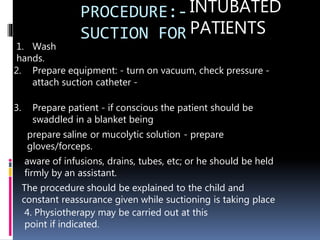
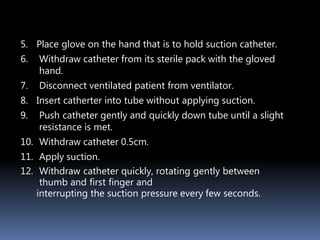
Suctioning is used to remove secretions from intubated patients and those unable to cough effectively. It should be done as quickly, gently, and cleanly as possible to minimize trauma while only performing when necessary. All necessary equipment should be prepared, including sterile catheters, lubricant, and collection materials. Suctioning is indicated for audible secretions, changes in ventilator pressures or volumes, or before releasing a cuff. Risks include trauma, hypoxia, cardiovascular effects, and atelectasis, so suctioning time should be minimized and oxygenation supported. Proper technique depends on the site being suctioned and maintains sterility.