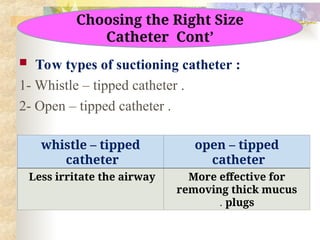
The document outlines the procedure and considerations for suctioning in pediatric nursing, including definitions, indications, catheter types, and equipment needed. It details the suctioning process for various sites, appropriate catheter sizes, and pressure settings for different age groups, along with documentation and monitoring requirements. Complications associated with suctioning, such as airway trauma and infection, are also highlighted.