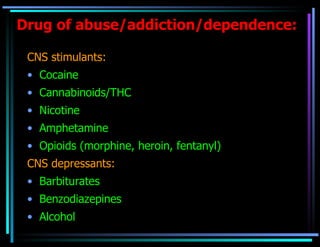
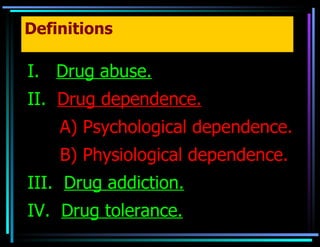
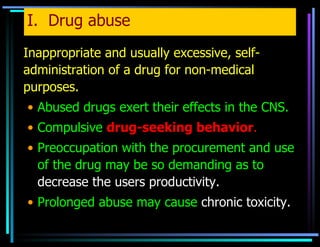
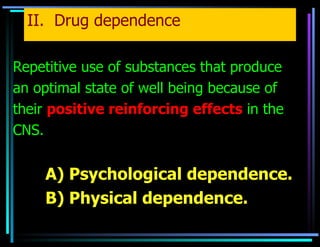
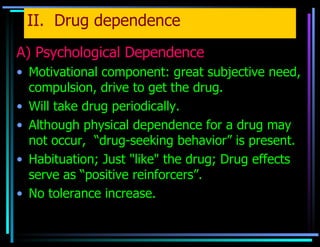
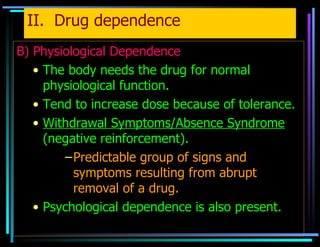
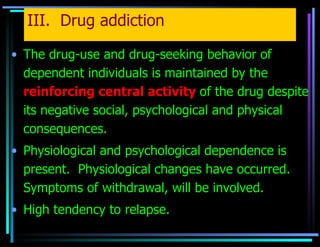
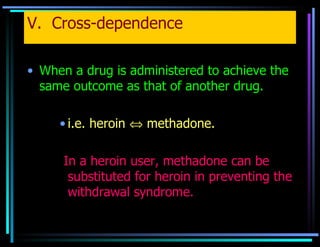
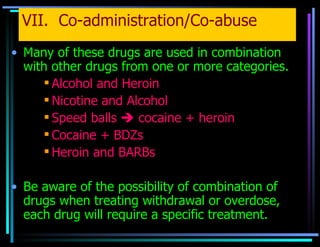
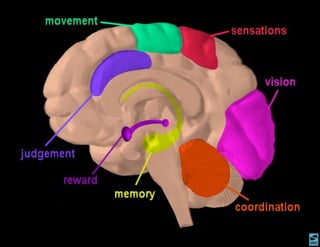
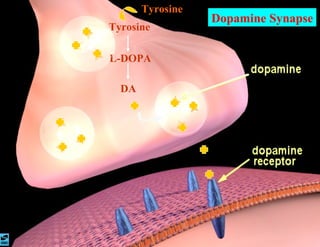
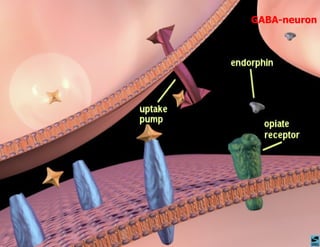
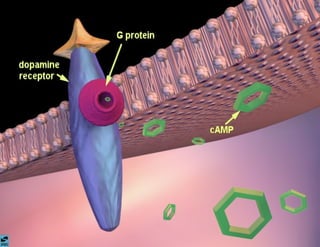
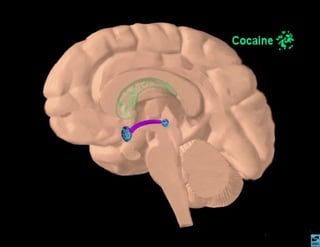
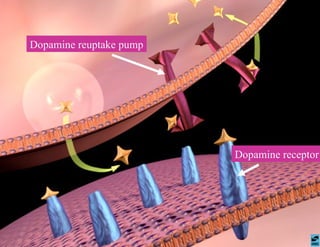
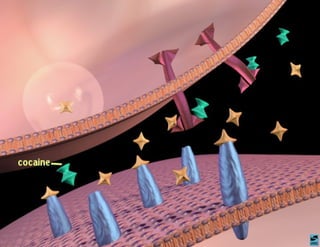
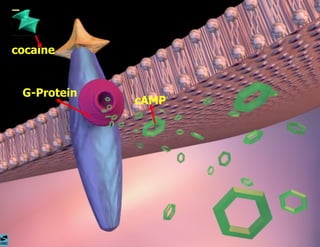
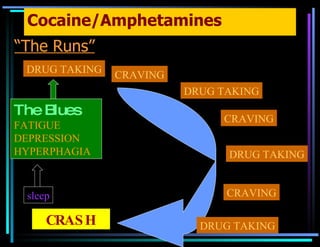
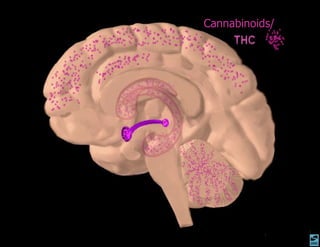
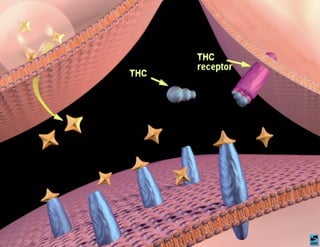
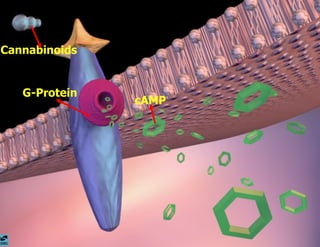
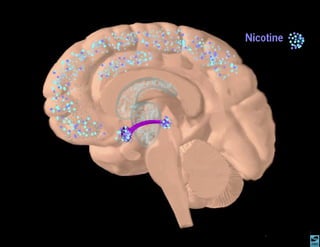
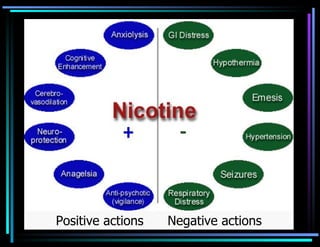
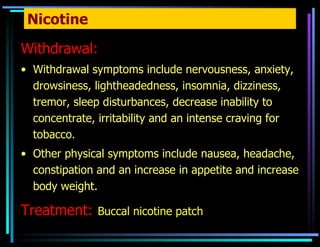
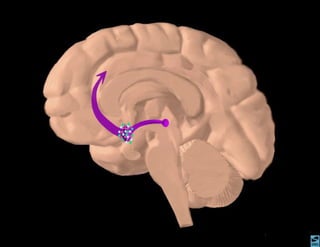
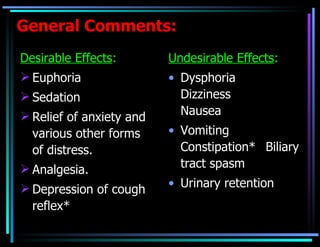
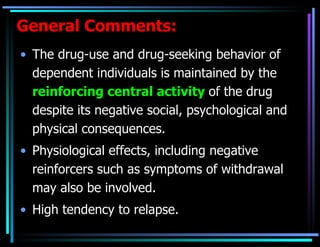
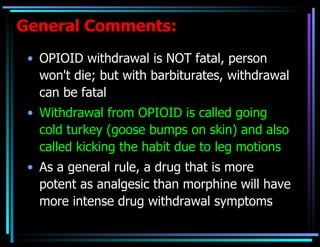
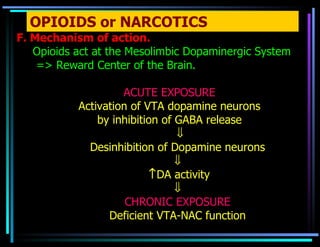
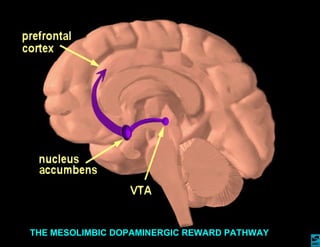
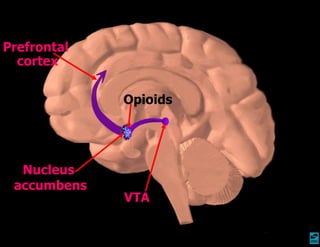
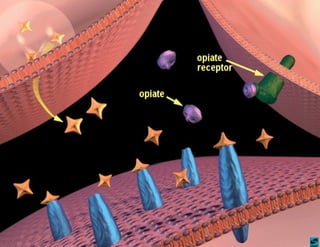
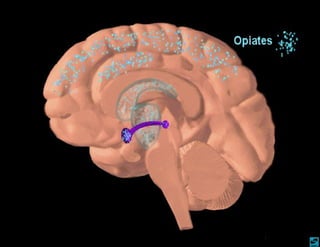
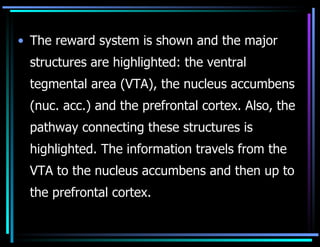
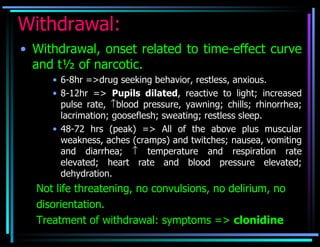
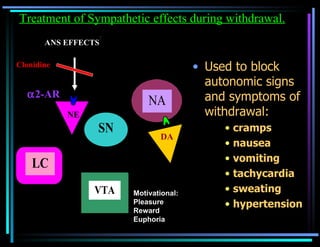
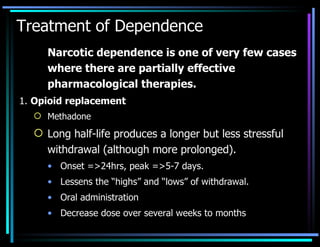
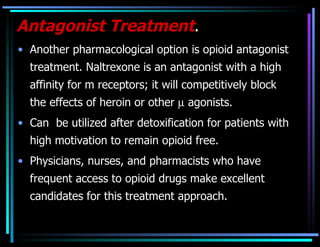
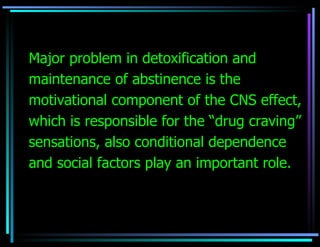
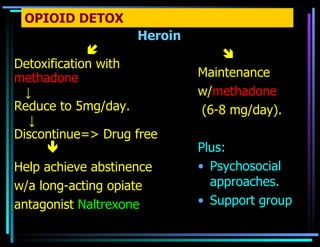
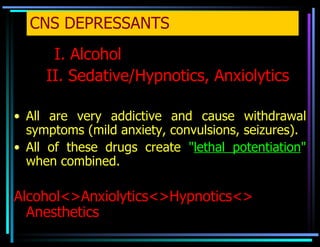
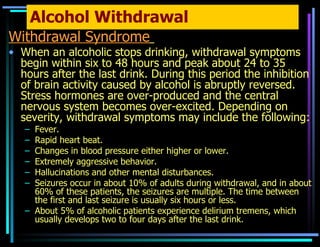
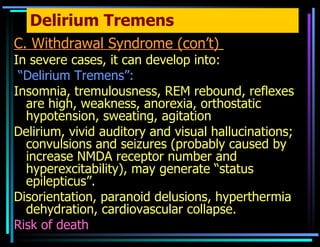
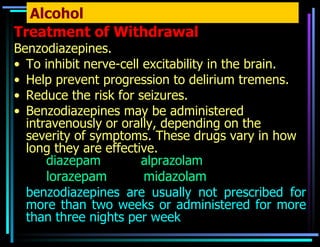
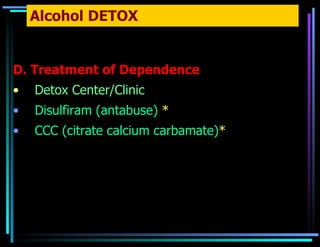
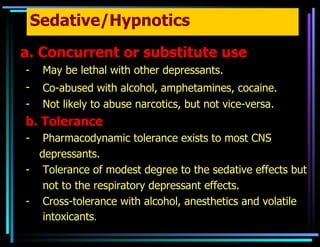
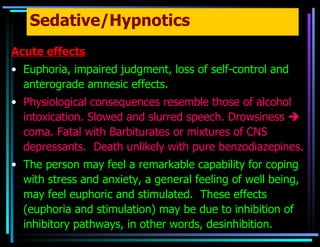
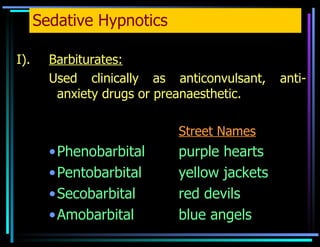
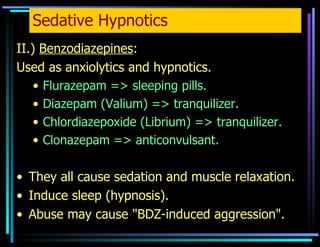
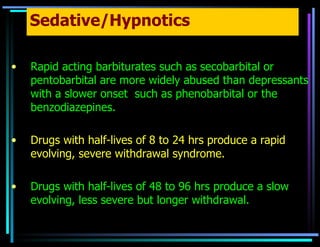
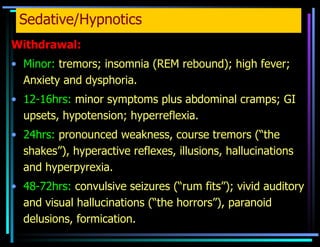
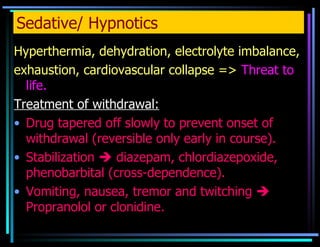
The document summarizes various drugs of abuse including their mechanisms of action, effects, dependence, tolerance, withdrawal and treatment approaches. It discusses stimulants like cocaine and amphetamines, opioids, cannabinoids, nicotine, depressants like alcohol, barbiturates and benzodiazepines. It describes how these drugs activate the brain's reward system and how chronic use leads to tolerance and dependence characterized by drug-seeking behavior and withdrawal symptoms when use is discontinued. Treatment involves managing withdrawal symptoms, replacing opioids with longer-acting alternatives, and addressing psychological aspects through counseling and support groups.