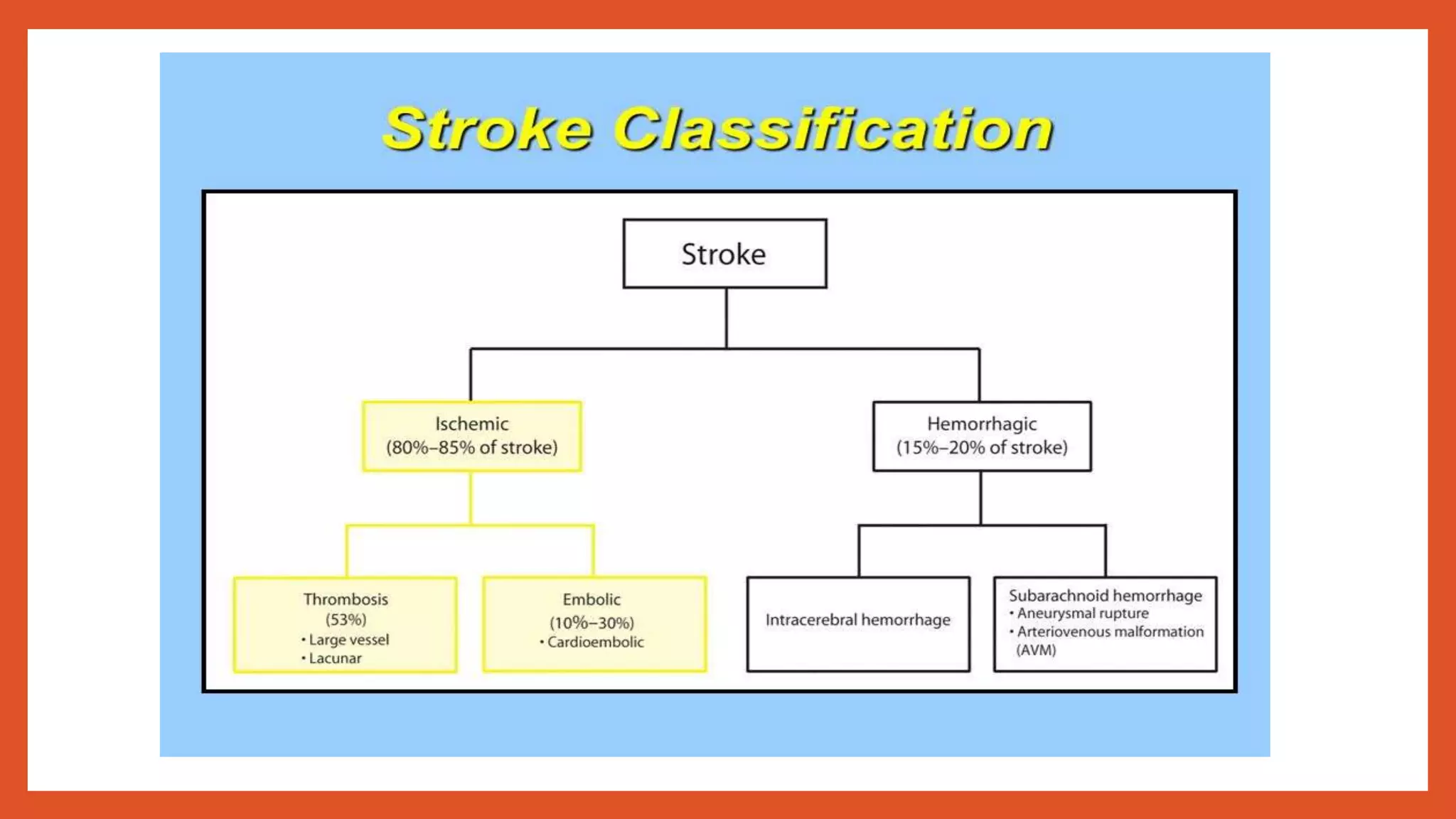
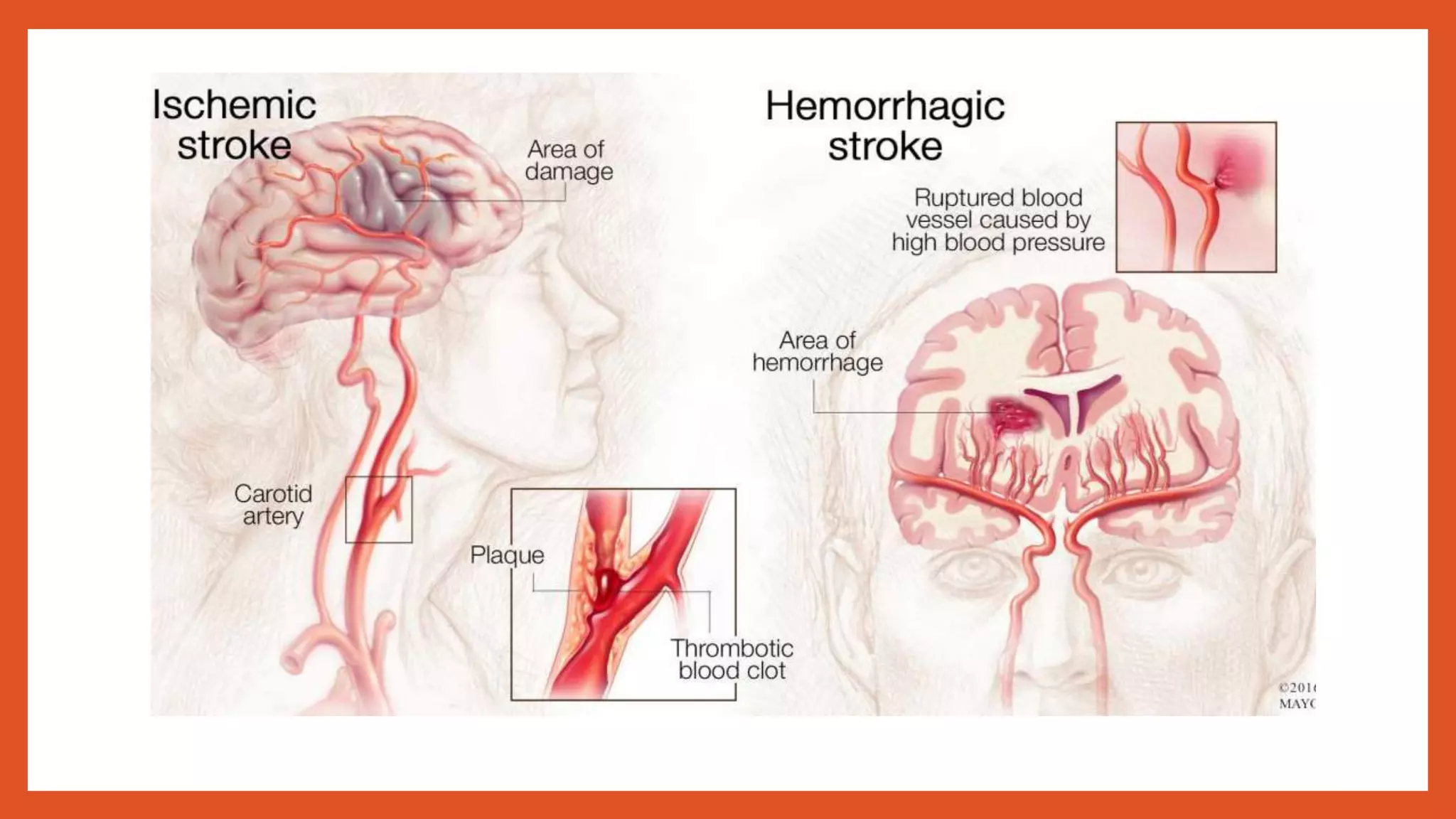
The document provides an overview of strokes, detailing their occurrence due to interrupted blood flow to the brain, classification, risk factors, pathophysiology, clinical manifestations, diagnosis, and management strategies. It distinguishes between ischemic and hemorrhagic strokes, outlining their causes and treatment options, including medication and surgical interventions. Additionally, it emphasizes the importance of secondary prevention through lifestyle changes and medical management.