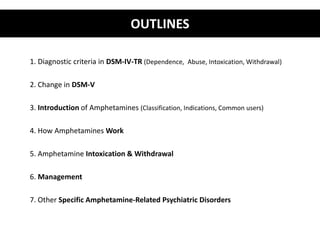
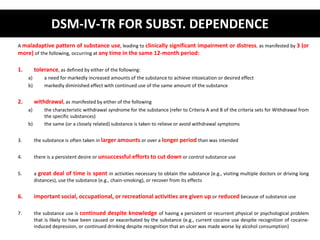
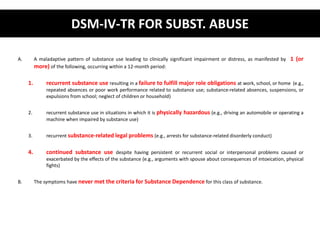
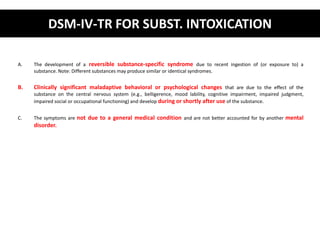
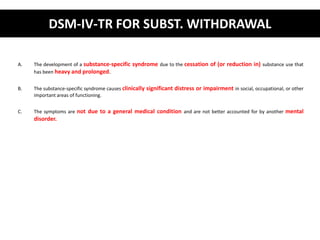
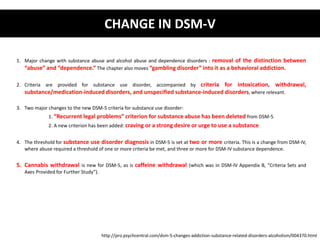
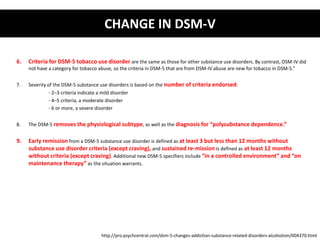
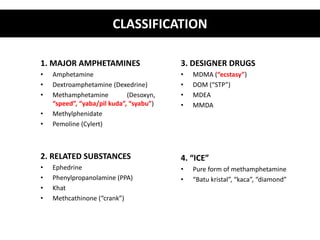
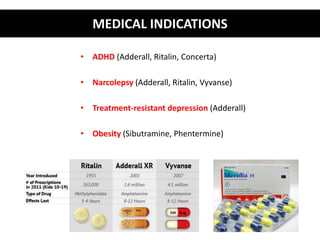
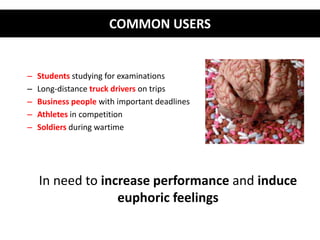
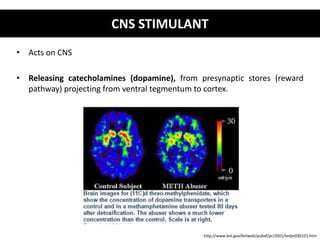
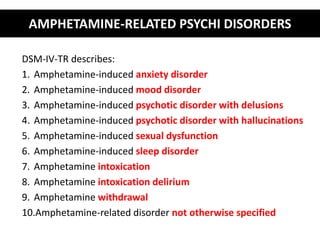
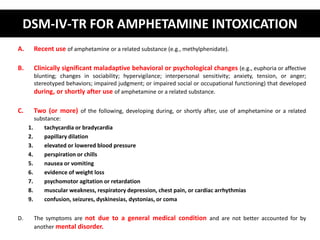
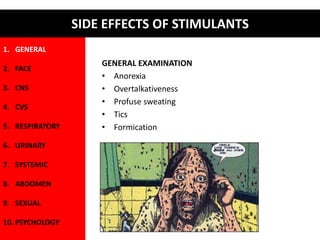
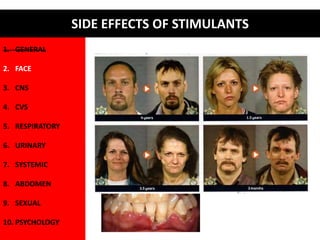
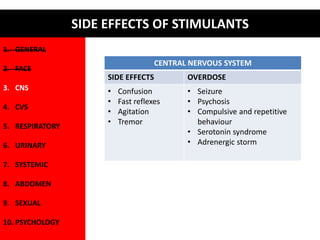
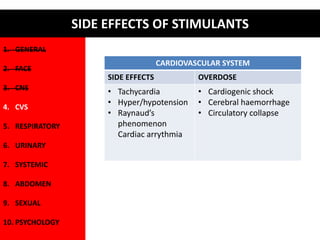
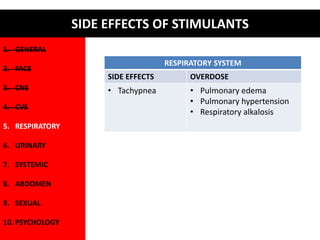
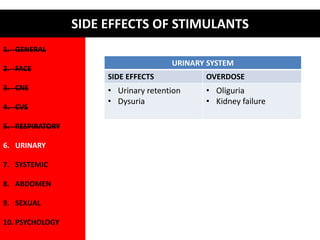
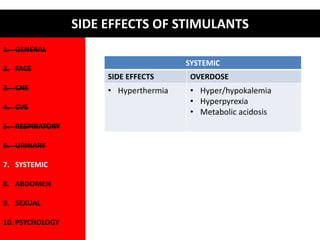
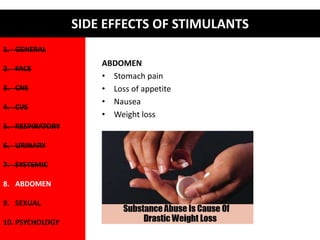
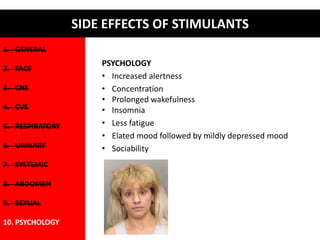
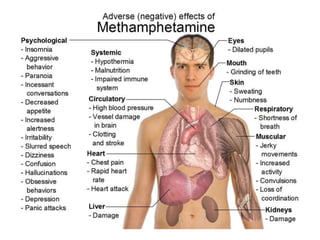
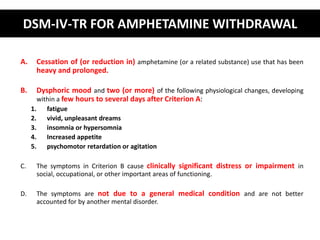
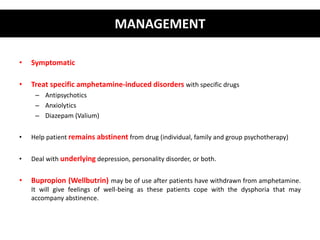
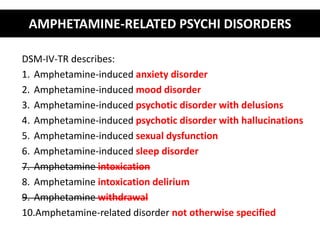
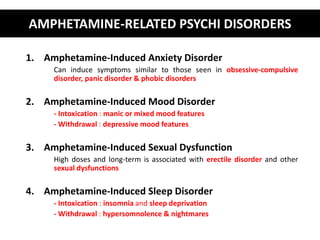
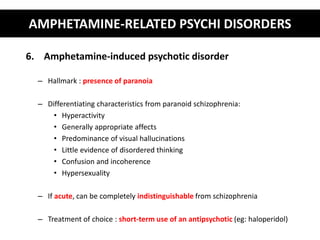
The document provides a comprehensive overview of substance-related psychiatric disorders, focusing on amphetamines, including diagnostic criteria from DSM-IV-TR and DSM-5, changes in definitions and classifications, and common disorders associated with amphetamine use. It discusses the management of amphetamine intoxication and withdrawal, emphasizing the need for symptomatic treatment and psychotherapy. Additional sections detail the effects of amphetamines, common user demographics, and the relationship between amphetamines and various psychiatric disorders.