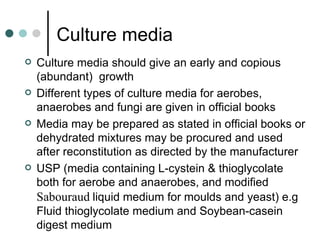
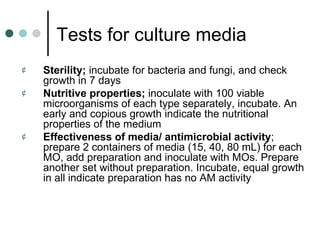
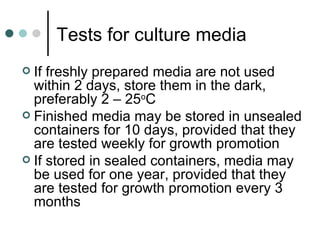
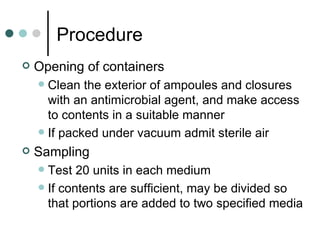
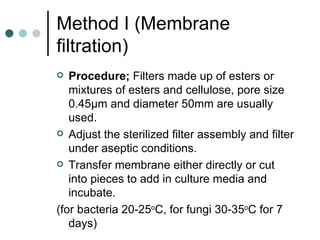
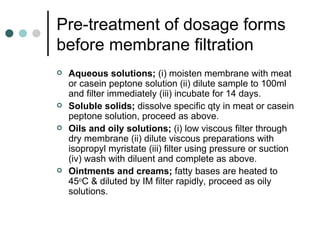
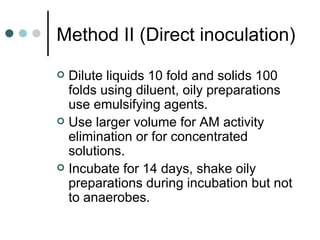
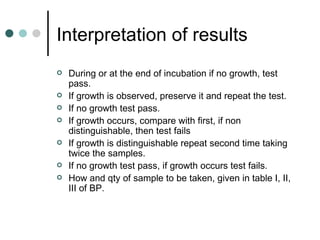
Sterility testing is required for all products labeled as sterile to ensure they have been effectively sterilized. Tests are conducted using specific culture media and procedures to detect any viable bacteria, fungi, or yeasts. The USP outlines sterility testing methods for various pharmaceutical products and devices, including membrane filtration and direct inoculation. Interpretation of results involves incubating samples and checking for any microbial growth over time, with growth indicating test failure.