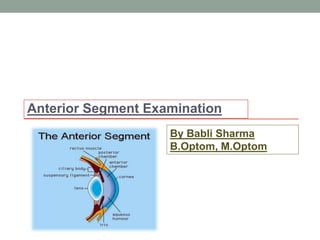
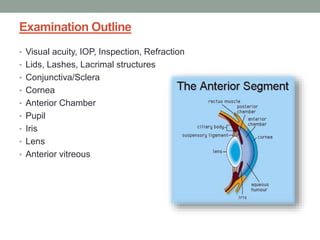
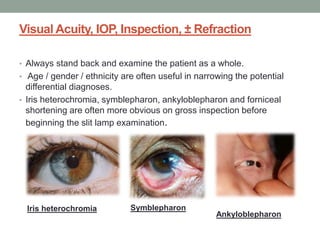
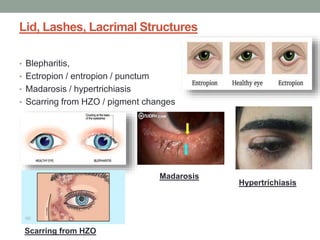
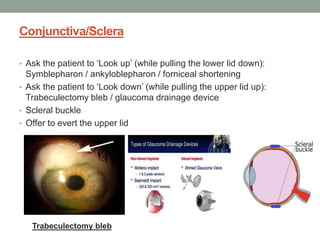
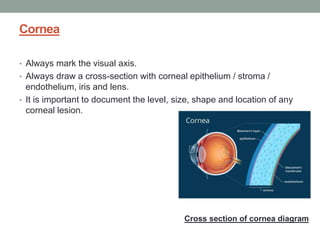
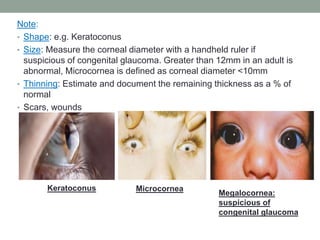
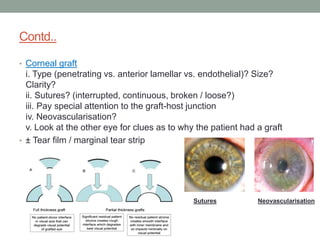
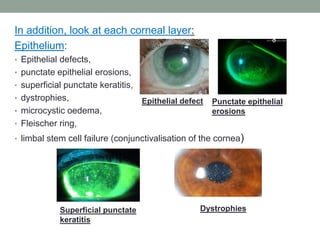
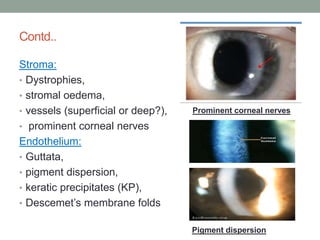
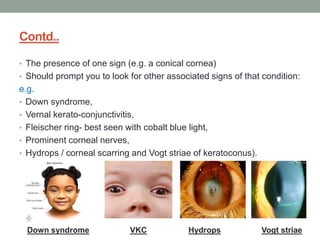
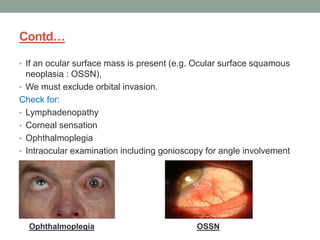
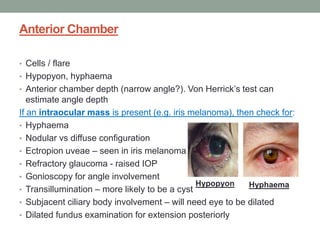
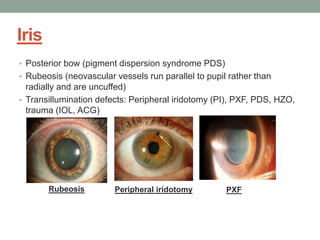
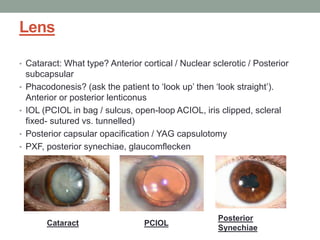
The document outlines a comprehensive approach to anterior segment examination, detailing key examination elements such as visual acuity, intraocular pressure, and inspection of various ocular components including the eyelids, conjunctiva, cornea, and lens. It emphasizes the importance of thorough visual assessment and documentation of findings, particularly in identifying conditions like keratoconus and ocular surface neoplasia. Additionally, it discusses relevant investigative methods that may be employed based on clinical findings.