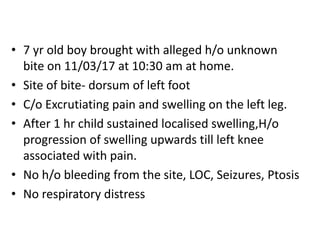
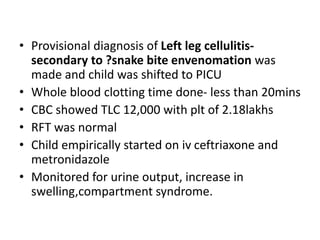
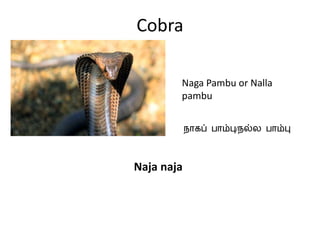
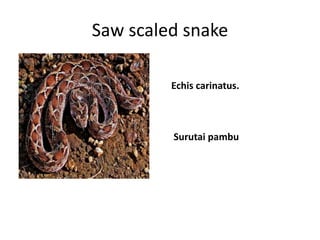
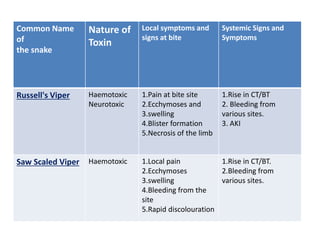
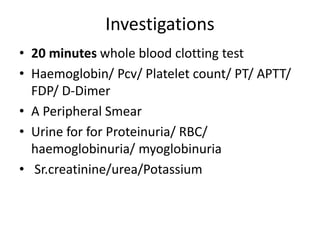
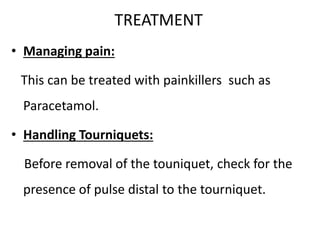
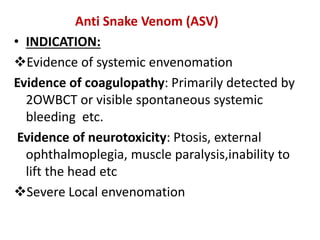
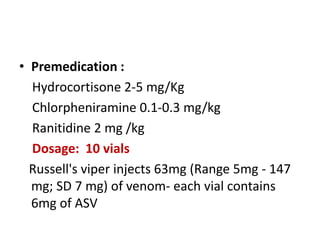
This document presents a case study of a 7-year-old boy who was bitten by a snake on his left foot. He experienced swelling and pain that progressed up his left leg. He was initially treated with IV fluids, analgesics, and antivenom at a local hospital before being referred for possible antivenom allergy.
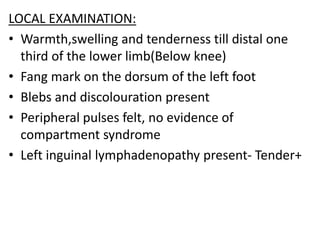
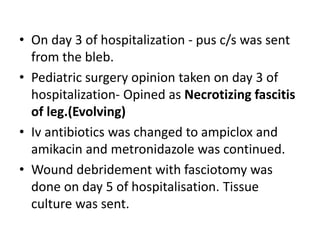
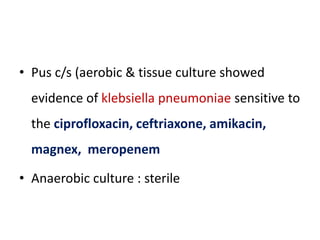
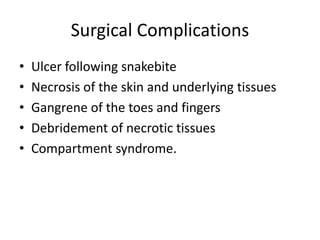
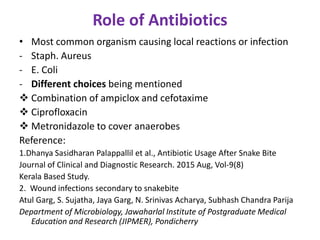
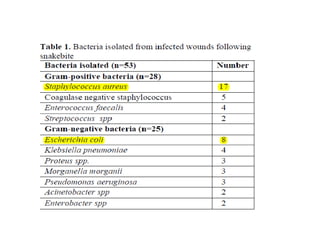
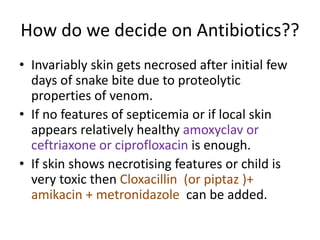
On examination, he had swelling up to his knee with tenderness and blebs. Investigations showed elevated white blood cell count. He developed worsening swelling and pus, and was diagnosed with necrotizing fasciitis. He underwent wound debridement and antibiotics were changed. Cultures grew Klebsiella pneumoniae. He was treated surgically and with antibiotics.