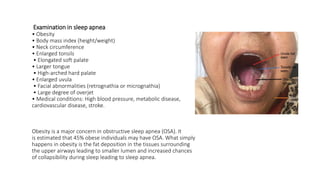
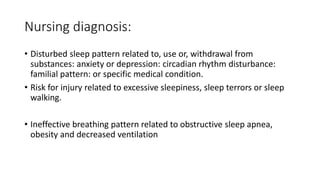
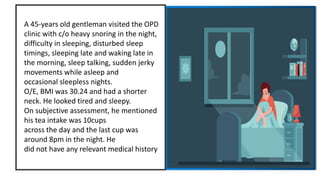
A 45-year-old man presented with sleep disturbances including heavy snoring, difficulty sleeping, and sleep talking, compounded by a high caffeine intake. His BMI of 30.24 suggests possible obesity-related sleep apnea, and the assessment indicates a need for further examination of his sleep patterns and possible insomnia or hypersomnia. Recommendations for management include a thorough medical history, sleep hygiene education, and potential lifestyle modifications.
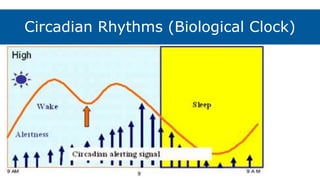
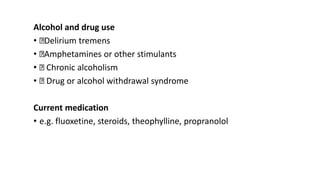
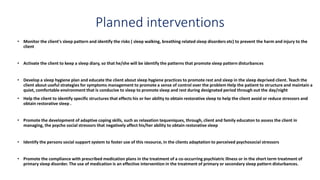
![Neuro-chemical influences on circadian
rhythm [sleep – wake cycle]:
Serotonin • Induction of sleep
Serotonin &
Norepinephrine
• Non-REM Sleep
Acetylcholine • REM
GABA • Regulation of sleep & arousal
Histamine • Prolongs REM Sleep](https://image.slidesharecdn.com/susmitamentalsleep-220719124925-ea516273/85/Sleep-Disorders-15-320.jpg)
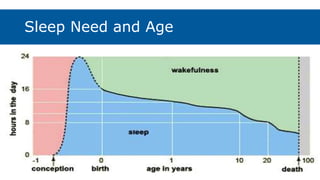
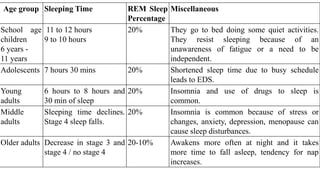
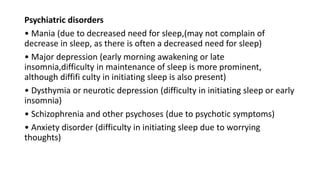
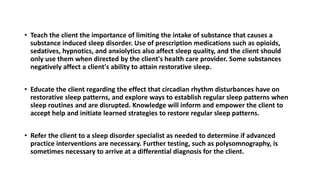
![Age group Sleeping Time REM Sleep
Percentage
Miscellaneous
Neonates 16 hours of sleep a day, sleeping
almost constantly during 1st
week, sleep cycle is generally 40
to 50 min
50% as it
stimulates
higher brain
function
Awakening occurs after 1 or 2 sleep cycles.
Infants [after 3
months]
Several naps during day, sleeps 8
to 10 hours at night with total 15
hours sleep.
30% Awakening commonly occurs early in the morning but can
awake at night also.
Toddlers By age 2, children usually sleep
through night and take daily
naps. After 3 years, usually give
up daytime naps. Total sleep
almost 12 hours a day.
20% Common to awaken at night. Toddler may unwilling to go to
bed at night due to a need for autonomy or a fear of
separation from their parents.
Pre – schoolers 12 hours 20% The pre-schoolers usually have difficulty relaxing or quieting
down after long, active days and has problem with bedtime
fears, waking during the night or nightmares. Partial
awakening followed by normal return to sleep is common. In
waking period, the child exhibit crying, walking around,
unintelligible speech, sleep walking or bed wetting.](https://image.slidesharecdn.com/susmitamentalsleep-220719124925-ea516273/85/Sleep-Disorders-17-320.jpg)